Acute pancreatitis
On abdominopelvic CT
Introduction
When it comes to imaging pancreatitis, timing is key. If a patient has upper abdominal pain and an amylase over three times the normal level, that’s usually enough to make the diagnosis. So why scan at all?
This article covers when to image, what to look for, and how to assess severity with CT. From finding gallstones to spotting necrosis and complications, it’s a practical guide to managing pancreatitis on imaging.
Case introduction
A male in his 50s presents with upper abdominal pain and has a CT abdomen and pelvis with IV contrast.
Have a look at the scan below.
I know you want to get going but you may need to wait a few seconds for the scan to load. Tap the first icon on the left to scroll.
Imaging findings
The main finding here is significant fat stranding within the upper abdomen – we can see this is centred on the pancreas suggesting there is acute pancreatitis.
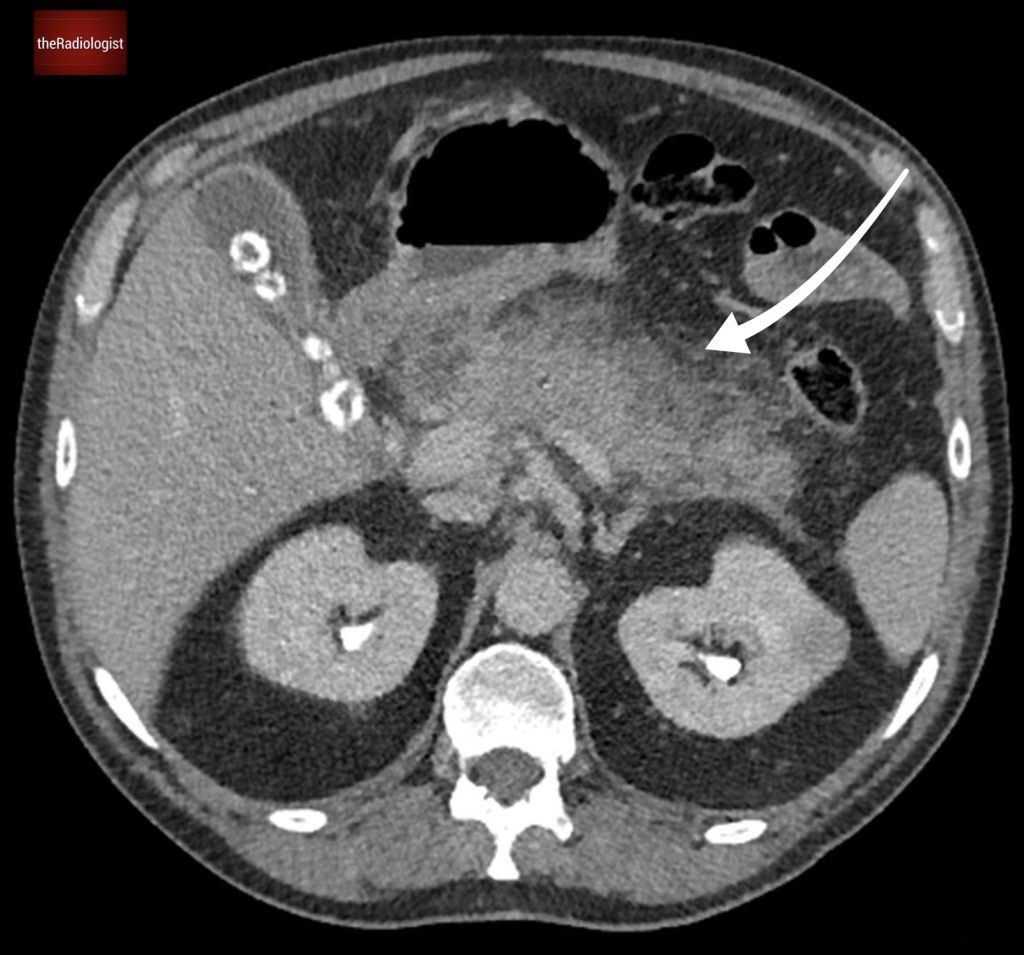
Fat stranding surrounding the pancreas.
Once you see there is pancreatitis firstly think about the cause. The two big causes are alcohol use and gallstones. CT is not fully sensitive for picking up gallstones but can see gallstones about 75% of the time so it is worth checking for. In our case we can clearly see calcified stones within the gallbladder suggesting this is acute pancreatitis secondary to gallstones. Once you see the stones also check for biliary dilatation however here the bile ducts have a normal calibre.
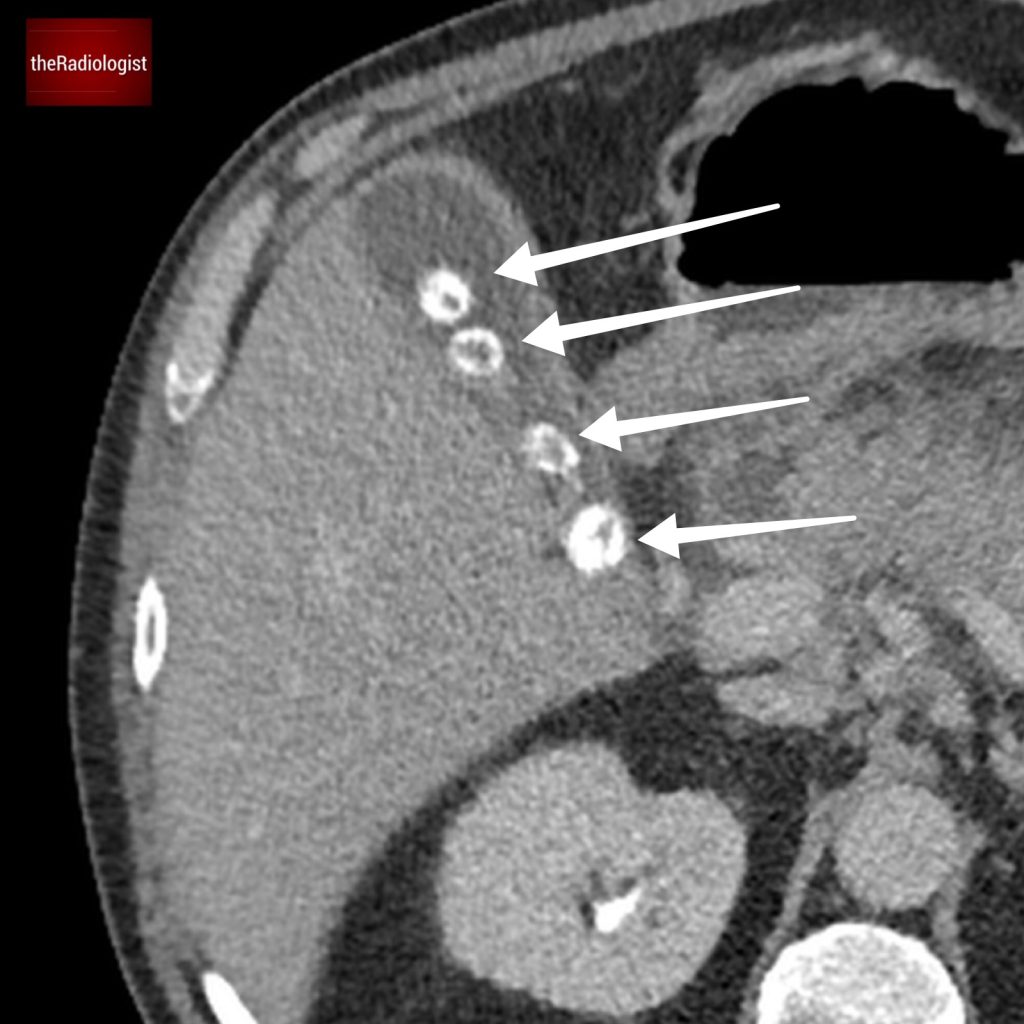
Calcified gallstones within the gallbladder. Have a look at the gallbladder wall – it is thin. More than 3 mm and you would consider cholecystitis.
Complications
Now we know the cause look for complications of pancreatitis:
- Look to see if all of the pancreas enhances. If it doesn’t there could be necrosis. This usually starts at least 3 days after the onset of symptoms and in the very early stages oedema can also cause reduced enhancement which is why CT may not always be helpful in the very early stage of pancreatitis.
- Look for discrete peripancreatic fluid collections.
- Assess the splenic vein, main portal vein and superior mesenteric vein looking for filling defects that could represent thrombosis.
- Assess the splenic artery looking for focal dilatation which could represent a pseudoaneurysm. This is better done on an arterial phase scan (the one we have is a portal venous although it is worth checking on this).
Imaging strategy
When it comes to imaging acute pancreatitis, timing is everything. An amylase level over 3 times the normal level in the context of acute upper abdominal pain is usually considered diagnostic for acute pancreatitis so why image at all?
- Looking for the cause of pancreatitis, ie gallstones in a large proportion of cases. Ultrasound is considered more sensitive than CT but CT can still pick up around three quarters of cases if not more.
- Confirming pancreatitis when the amylase may be borderline or there are other complicating factors in the history.
- To look for complications.
- To assess severity.
In the UK it is not usual practice to image in the first 3 days of symptom onset as this may underestimate the degree of pancreatic necrosis. The presence of necrosis can be an important prognostic factor particularly if affecting the head of the pancreas. There are several scoring systems when it comes to stratifying severity of acute pancreatitis but let’s look at the ‘modified CT severity index’ (CTSI) which is a little more simple than the CTSI itself.
MODIFIED CT SEVERITY INDEX
Calculate the total number of points and feed into the table below:
Inflammation
0: Normal pancreas
2: Intrinsic pancreatic abnormalities
4: Pancreatic/peripancreatic fluid collection or fat necrosis
Necrosis
0: None
2: ≤30%
4: >40%
Extra-pancreatic complications
2: pleural effusion, ascites, vascular, parenchymal or GI involvement
| Total score | Severity |
|---|---|
| 0-2 | Mild |
| 4-6 | Moderate |
| 8-10 | Severe |
Incidental finding
Looking elsewhere on the scan there is also an incidental finding of a small soft tissue lesion relating to the left kidney. Notice this does not show the normal density of a simple cyst (0-20 HU). The differential on this single phase CT includes a benign cyst with proteinaceous/haemorrhagic content or a soft tissue lesion such as an RCC.
The options in the first instance for further characterisation include ultrasound and a dual phase renal protocol CT. The lesion in this instance turned out to be a benign renal oncocytoma which can mimic renal cell carcinoma.
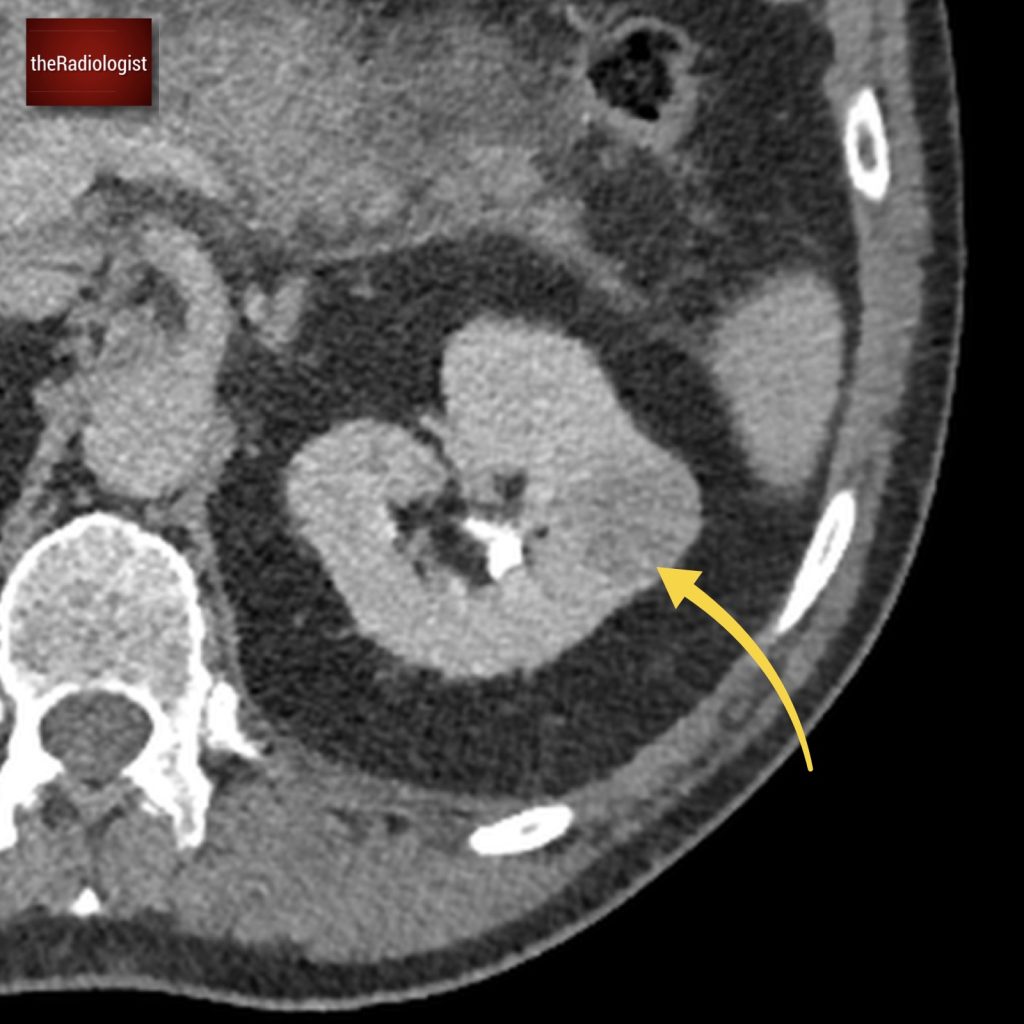
Soft tissue density lesion related to the left kidney, does not appear like a simple renal cyst.
KEY POINT
After 72 hours is usually the optimal time for CT in the context of acute pancreatitis. US looking for gallstones can be performed at any time.
If there is duct dilatation on US an MRCP may help looking for obstructing CBD stones. Repeat CT imaging can be performed to follow up complications.