Shoulder dislocation
On X-Ray
Introduction
A male in his 80s presents with shoulder pain after trauma and the X-Ray shows a common injury with key imaging signs to know.This quick case review covers how to assess a shoulder X-ray for dislocation, associated fractures, and classic features like Hill-Sachs and Bankart lesions.
Case introduction
A male in his 80s presents to the Emergency Department with shoulder pain and deformity after an episode of trauma. Have a look at the X-Ray below, what does it show?
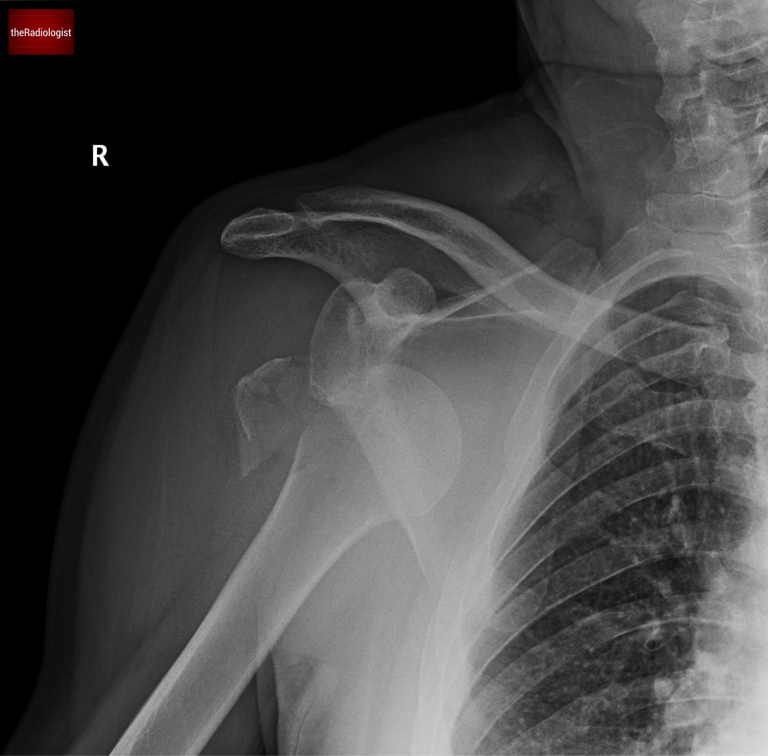
AP view of a shoulder X-Ray: what is the abnormality?
Assessing for a fracture
The first issue here is to notice that the proximal humerus is fractured – we can see the greater tuberosity has completely come apart from the humeral head! This means there has been a displaced fracture.
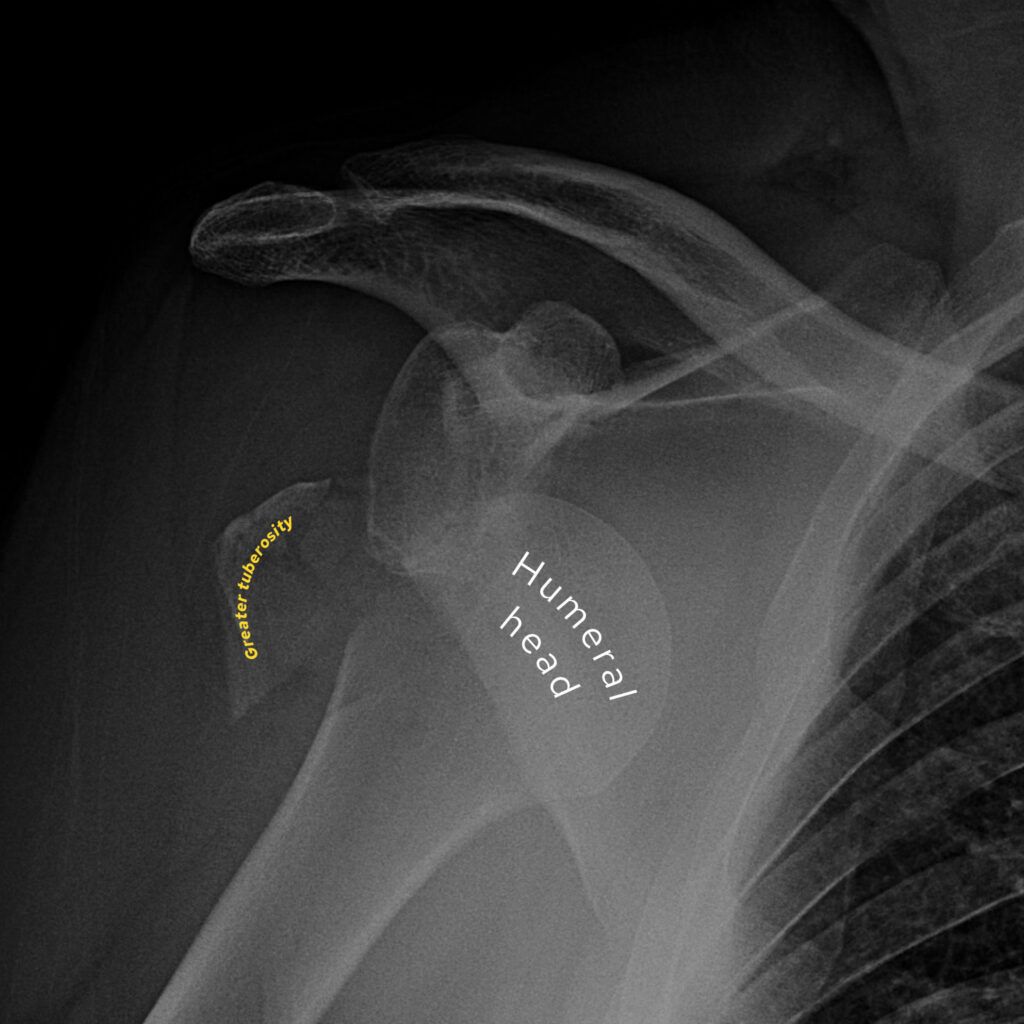
The greater tuberosity has come apart from the humeral head.
Assessing for dislocation
It is important not to stop there – as always it’s important to follow your normal review patterns. On all shoulder X-rays alignment of the glenohumeral joint should always be high up on your list of things to check. Try and outline the glenoid which is part of the scapula and on an AP view is ‘oval shaped’. Look to see if the humeral head lines up with this and sits next to the ‘oval’...
In our case we can see the humeral head has come away from the glenoid and looks like it has moved towards the ribs. This is typical for an anterior dislocation. Have a look at the post surgical film below- the humerus now sits next to the glenoid.
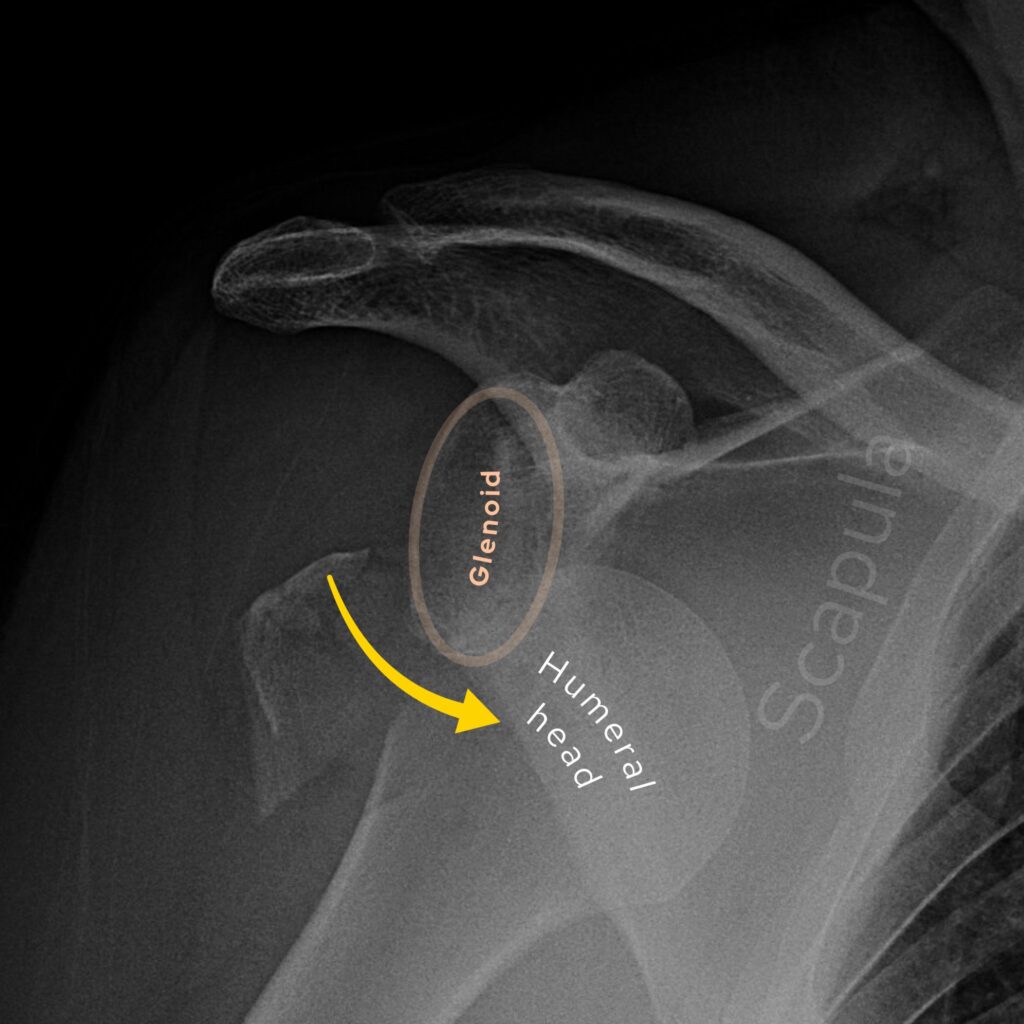
The humeral head does not line up with the glenoid and moves towards the ribs – typical for an anterior dislocation.
It is usual practice to look to try and get two views of the shoulder in cases of trauma although that can be tricky if the patient is in a lot of pain. There are different options for the supplementary view to the AP, with commonly used views including the ‘Y view’ and the ‘modified axial view’.
Posterior dislocations can be a lot more challenging to diagnose on X-ray. These are less common and are classically associated with seizures given the shoulder is pushed posteriorly in internal rotation whilst the arm is abducted. On X-ray, rather than appearing like the head of a walking stick, the humeral head has a ‘lightbulb appearance’.
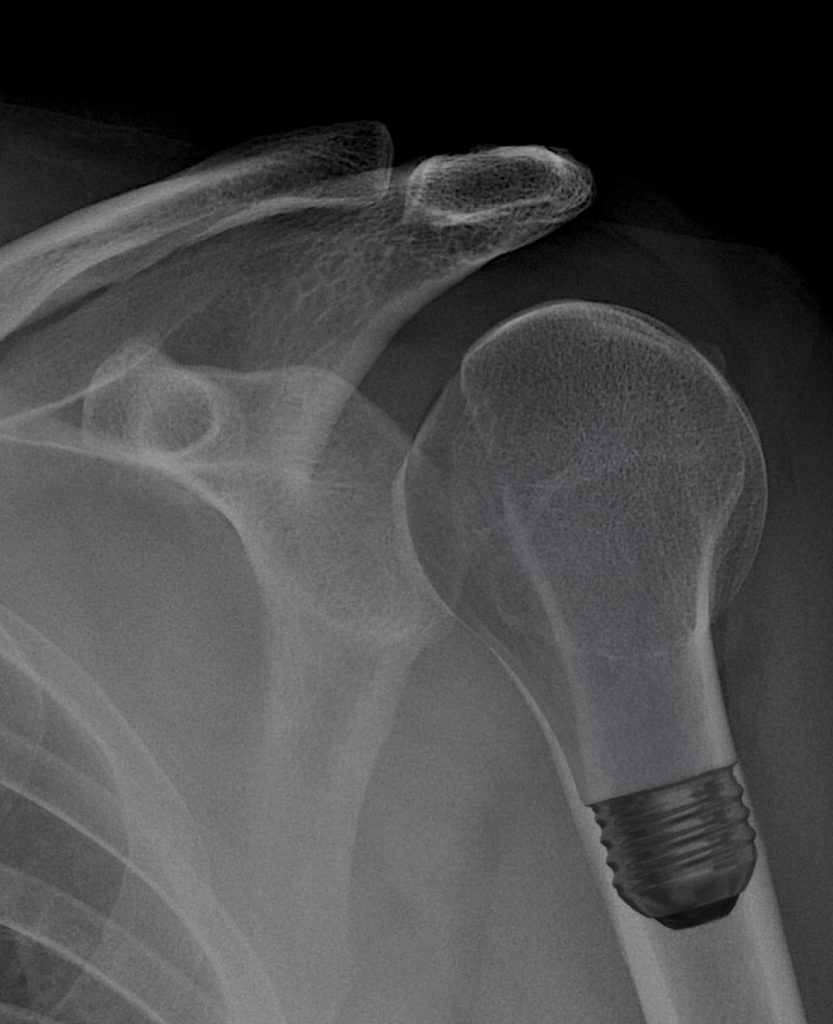
In a posterior dislocation look for a ‘lightbulb appearance’ of the humeral head.
Anterior shoulder dislocation
Anterior shoulder dislocation is the most common type of shoulder dislocation, accounting for over 95% of cases. It occurs when the humeral head is displaced anteriorly out of the glenoid fossa, usually due to trauma or excessive abduction and external rotation. Quick diagnosis and management are important to prevent complications such as recurrent instability, neurovascular injury, and chronic pain.
Common mechanisms include falling onto on outstretched hand or direct impact. As well as seeing the humeral head move towards the ribs on an AP view, a second view like a ‘Y-view’ can help confirm the dislocation as the humeral head does not line up with the glenoid.
The dislocation can be associated with Hill-Sachs or Bankart lesions.
1. Hill-Sachs lesion
A compression fracture of the posterolateral humeral head caused by impaction against the anterior glenoid during dislocation. It is best seen on AP and axial views. Larger lesions increase the risk of recurrent dislocations and may require surgical intervention.
2. Bankart lesion
A detachment of the anterior-inferior labrum from the glenoid, often accompanied by an injury to the glenoid bone (bony Bankart). The bony injury may be seen on X-Ray but you will probably need a CT or MR arthrogram. This lesion contributes to shoulder instability and may necessitate surgical repair in younger, active individuals.
KEY POINT
Remember to check the alignment of the glenoid and humeral head on every shoulder X-Ray you look at.
Posterior dislocations can be more challenging to pick up and you are looking for a ‘lightbulb’ appearance of the humeral head.