Multiple lung nodules
On chest X-Ray and CT
Introduction
A 40-year-old woman presents with chest pain and is found to have multiple lung nodules on X-Ray.
What do you do next, and how do you narrow down the differential?
This case takes you step by step through chest X-Ray and CT interpretation, the key features of multiple lung nodules, how to approach the differential, and what to do when imaging alone isn’t enough.
Case introduction
A 40 year old female presented to her local Emergency Department with chest pain and had a chest X-Ray. There was no significant known past medical history.
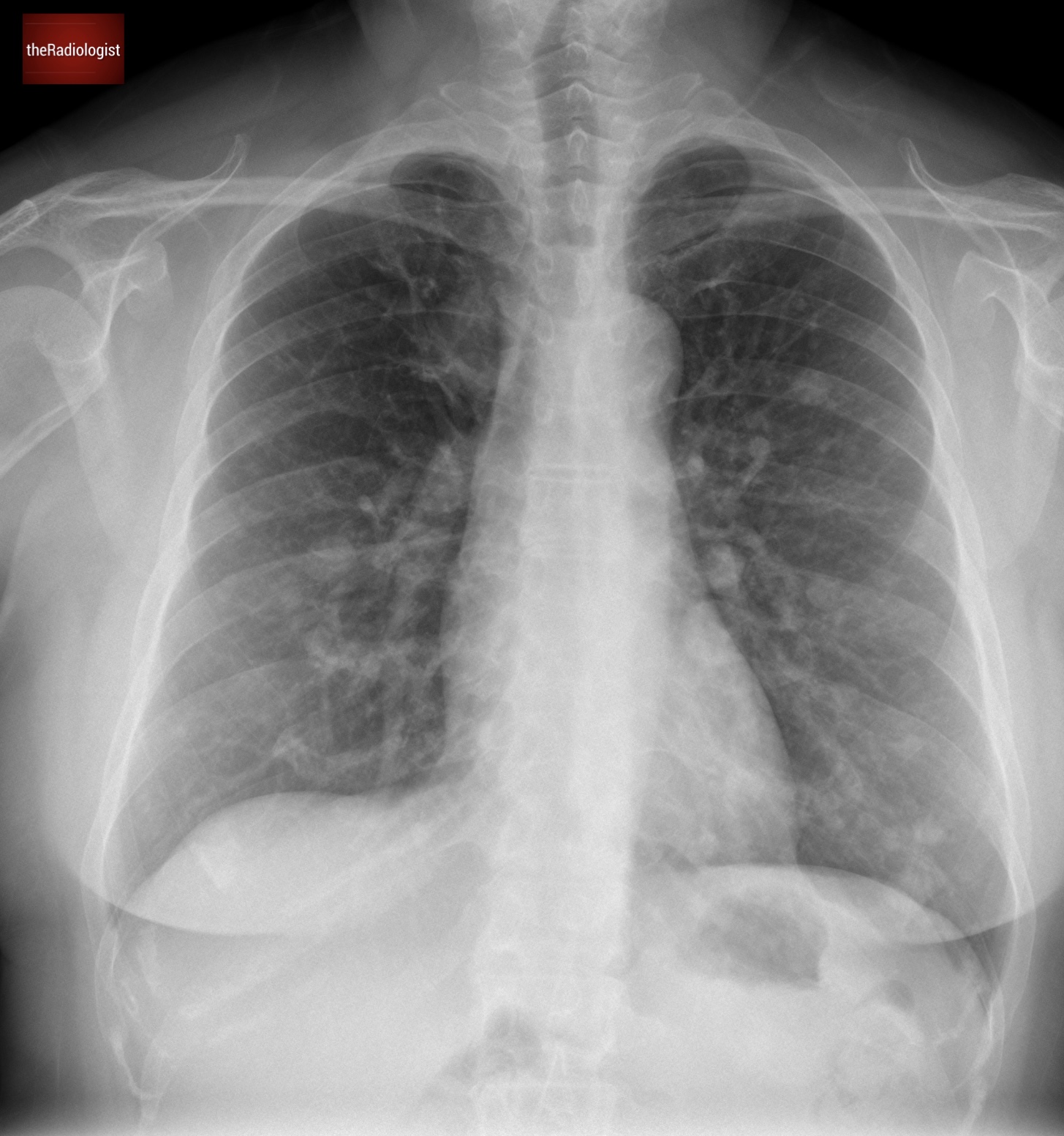
PA view of a chest X-Ray of a female in her 40s
Video explanation
Here is a video explanation of this case: click full screen in the bottom right corner to make it big. If you prefer though I go through this in the text explanation below.
Initial findings
The X-Ray shows multiple lung nodules. On the left, there’s a distinct nodule in the upper zone, and another larger one overlapping the heart border. Moving to the right side, we see a similar pattern, with multiple nodules scattered throughout.
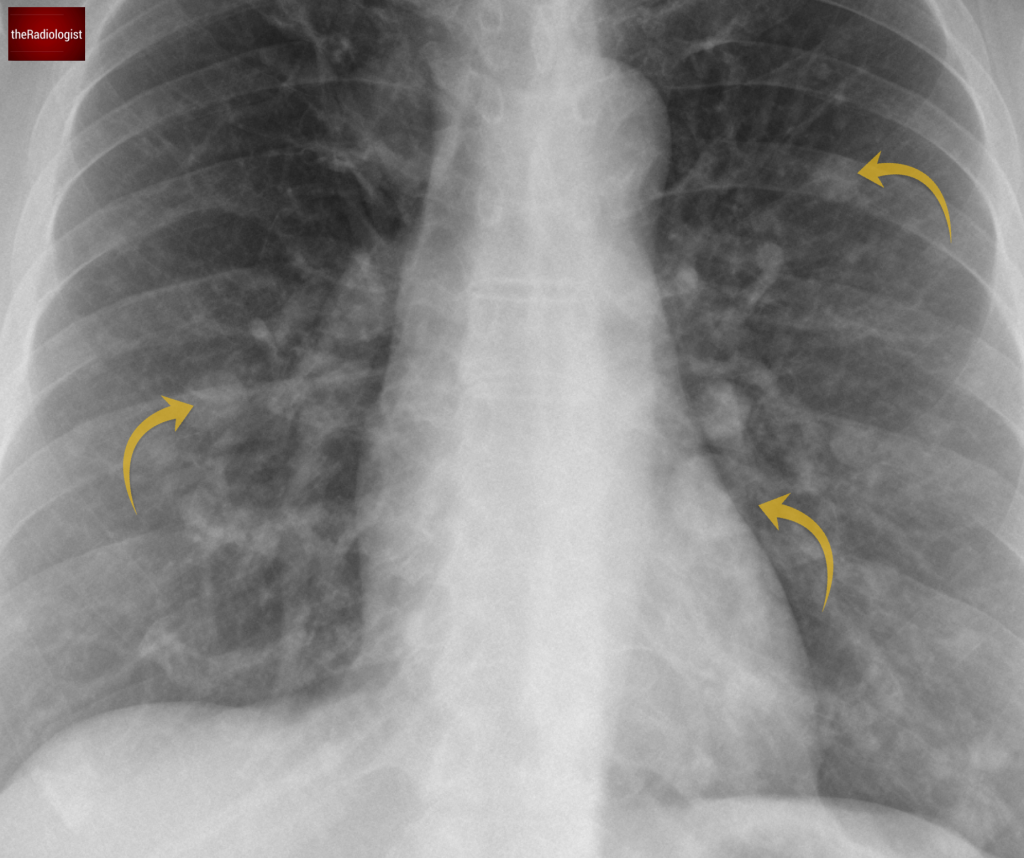
We can see several well defined lung nodules within both lungs.
Differential diagnosis for multiple lung nodules
What is the differential for multiple lung nodules on chest X-Ray in general?
Let’s break this up into different categories and go through it systematically.
| Category | Cause | Notes |
|---|---|---|
| Malignant | Metastases | Common cancers include from breast, colorectal, renal cell, thyroid, melanoma and gynaecological cancers. Will appear well circumscribed with a random distribution, sometimes more towards the lower lobes |
| Primary lung cancer | Multifocal adenocarcinoma can present as multiple solid or groundglass nodules | |
| Pulmonary lymphoma | Can present with multiple nodules, masses or consolidation | |
| Sarcoma | Uncommon cause | |
| Carcinoid | Pulmonary carcinoid usually presents as either an endobronchial lesion or well defined peripheral nodule but more rarely you may see multiple nodules associated with mosaic attenuation in a condition known as diffuse idiopathic pulmonary neuroendocrine cell hyperplasia (DIPNECH). | |
| Infection | Fungal | Including aspergillosis, histoplasmosis and coccidiodomycosis. |
| Mycobacteria | Including TB and NTM (non-tuberculous mycobacteria). Nodules may show cavitation. | |
| Viral | Including CMV or varicella. Multiple calcified nodules can indicate previous varicella pneumonitis. | |
| Septic emboli | You may see multiple small cavitating nodules and wedge shaped opacities. | |
| Inflammatory and autoimmune | Rheumatoid nodules | Usually peripheral, small and well defined. Can cavitate. |
| Granulomatosis with polyangiitis (Wegener’s) | Can cavitate. May present as multifocal consolidation and may see regions of pulmonary haemorrhage. | |
| Sarcoid | Small bronchocentric nodules, can present as larger ill defined ‘shaggy’ nodules. Look for nodules on the fissures on CT and symmetrical bilateral hilar and mediastinal nodes. | |
| Benign | Hamartoma | Usually solitary but occasionally can be larger |
| Benign metastasing leiomyomas | Seen in women with a history of uterine fibroids. Nodules are well defined and bilateral. | |
| Granulomata | Usually calcified so will look brighter on X-Ray. | |
| Vascular | AVM | Can be single. Look for a feeding vessel although this can be difficult to see on chest X-Ray. Multiple AVMs associated with hereditary haemorrhagic telangiectasia. |
| Infarcts | May see as wedge shaped opacities. Think about PE and septic emboli. | |
| Other | Pneumonicosis | You may see multiple nodules. Silicosis can look like sarcoid. |
| Amyloidosis | Range of presentations but you may see multiple partially calcified nodules. |
OK so that is a long list. Let’s now try and apply that to this case and narrow down the differential:
Malignancy
Lung metastases should always be on the radar and in essence multiple lung nodules are metastases till proven otherwise. In a younger female, potential primary sources include:
- Breast cancer
- Gynecological malignancies, such as cervical or endometrial cancer
Atypical infections
Fungal infections can sometimes cause discrete larger nodules, though this is uncommon. Septic emboli, which tend to produce smaller, peripheral nodules that may cavitate or form wedge-shaped opacities are also on the differential but we have nothing about fever or raised inflammatory markers in the clinical history.
Autoimmune and inflammatory conditions
Rheumatoid nodules: Typically small, peripheral, and well defined so worth thinking about.
Vasculitis: Granulomatosis with polyangiitis (formerly Wegener’s) should also be considered and so it is worth performing an ANCA screen.
Rare causes
Benign metastasizing leiomyomas: These are rare and specific to females with a history of uterine fibroids but something I usually consider in females of this age with multiple nodules of uncertain cause.
Investigations
A CT of the thorax, abdomen and pelvis with contrast was performed confirming the X-Ray findings of multiple bilateral well defined lung nodules of different sizes.
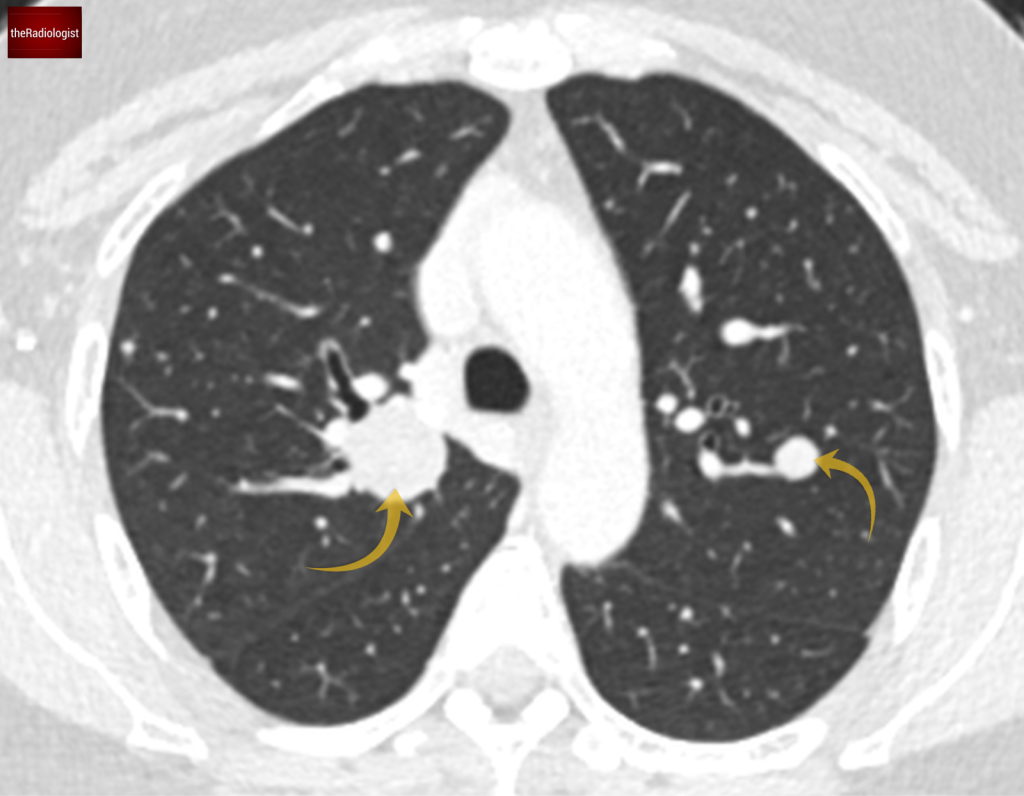
CT confirms several well defined nodules within both lungs.
The only additional significant finding was of an enlarged uterus suggesting the presence of uterine fibroids.
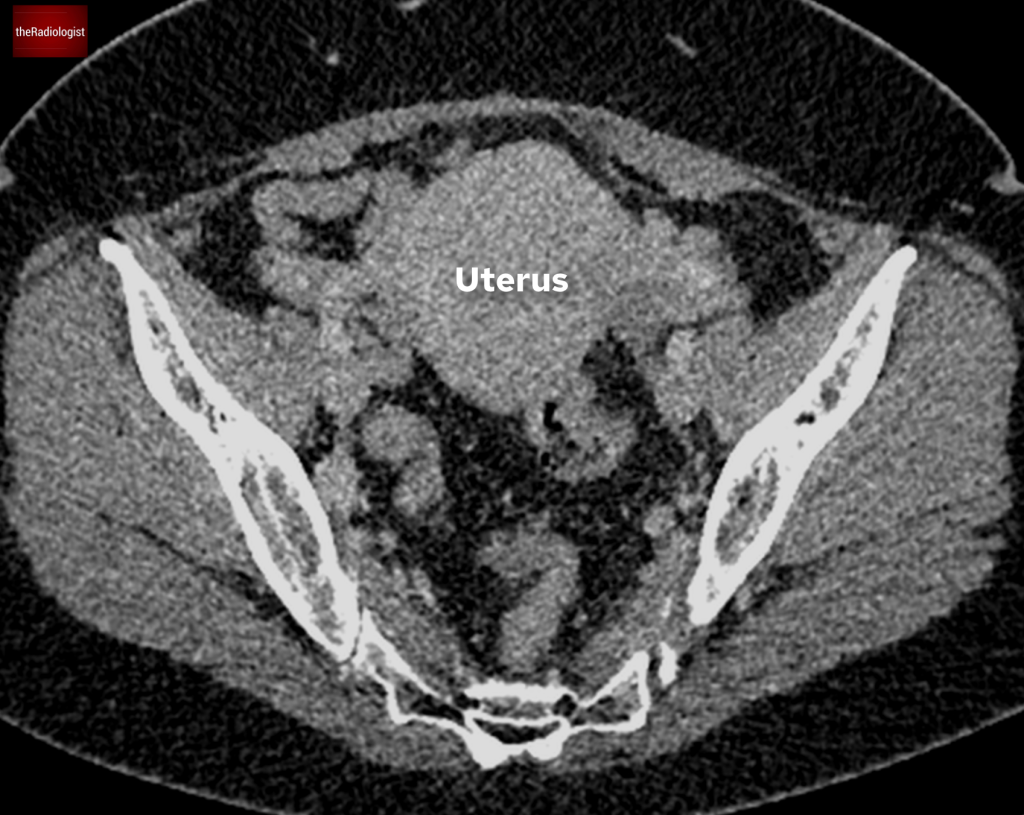
Body CT also showed an enlarged uterus.
Next came a PET-CT scan. While the lung nodules showed only mild FDG avidity, areas within both breasts exhibited more significant avidity. This prompted a referral to the breast unit for further investigation. The breast lesions turned out to be benign papillomas, unrelated to the lung nodules.
PET-CT shows only low grade FDG avidity within the lung nodules with high FDG avidity within several bilateral breast nodules, subseuqnetly worked up and found to represent benign papillomas.
To be certain of the diagnosis a CT-guided lung biopsy was performed which provided the answer: benign metastasising leiomyomas.

CT guided biopsy of a large right sided lung nodule was performed to obtain a tissue diagnosis of benign metastasising leiomyomas.
Benign metastasising leiomyomas
Benign metastasising leiomyomas (BML) is a rare condition where benign uterine fibroids (leiomyomas) metastasise to extrauterine sites, most commonly the lungs. The pathophysiology isn’t fully understood, but it’s thought to involve hematogenous spread.
- Presentation: Patients may be asymptomatic or present with symptoms like chest pain, cough, or breathlessness.
- Imaging features: Lung nodules in BML are typically well-defined, bilateral, and can measure up to several centimeters, with the surrounding lung appearing normal.
- Management: While lesions often remain stable or regress, hormonal manipulation, embolization, or surgery may be considered for symptomatic cases.
This condition differs from leiomyosarcoma, which is malignant and far more aggressive.
KEY POINTS
With multiple lung nodules it is important to create a differential diagnosis based on the patient demographics and clinical context. In some cases, like this one, lung biopsy is necessary to find out the cause.
It is a rare cause but in cases of lung nodules in younger females with fibroids and no other clear cause, it is worth considering benign metastasing leiomyomas.