Multiple cavitating lesions
How to approach on chest X-Ray and CT
Introduction
A man in his 80s presents unwell and his chest X-ray shows multiple lung lesions. When you see cavitation on imaging, especially when it’s widespread, the key is having a structured approach.
In this case, we break down how to recognise cavitation, work through the differential using the STARE mnemonic, and explore how to narrow things down with clinical context, CT findings, and biopsy.
A practical guide to tackling one of the more complex patterns in chest imaging.
Case introduction
When you’re faced with multiple cavitating lung lesions on imaging, it’s really important to approach the case methodically, as the differential diagnosis is broad – however it is manageable with a structured approach.
Let’s go through a case of a male in his 80s who presented unwell to the Emergency Department and had a chest X-Ray.
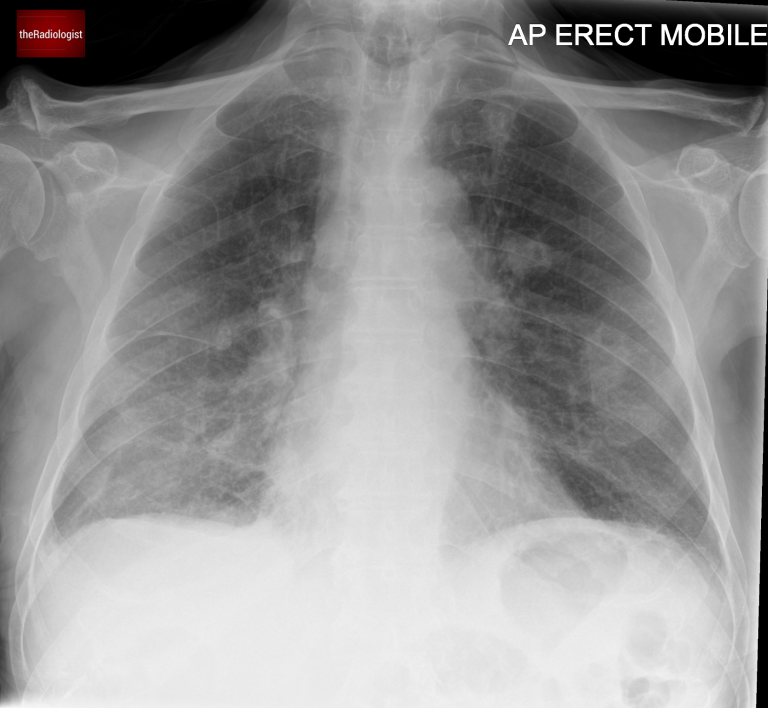
AP Chest X-Ray
Video explanation
Here is a video explanation of this case: click full screen in the bottom right corner to make it big. If you prefer though I go through this in the text explanation below.
Initial assessment
Here we have a non contrast CT KUB looking for renal tract calculi.
When we zoom in, we can see a bilateral abnormality. On closer inspection, some of these lesions have a small associated lucency, representing gas within the lesion.
This finding is called cavitation, and identifying it helps significantly narrow down the differential diagnosis. The differential changes as to whether we are dealing with either a single or multiple cavitating lesions. Let’s have a look at both below
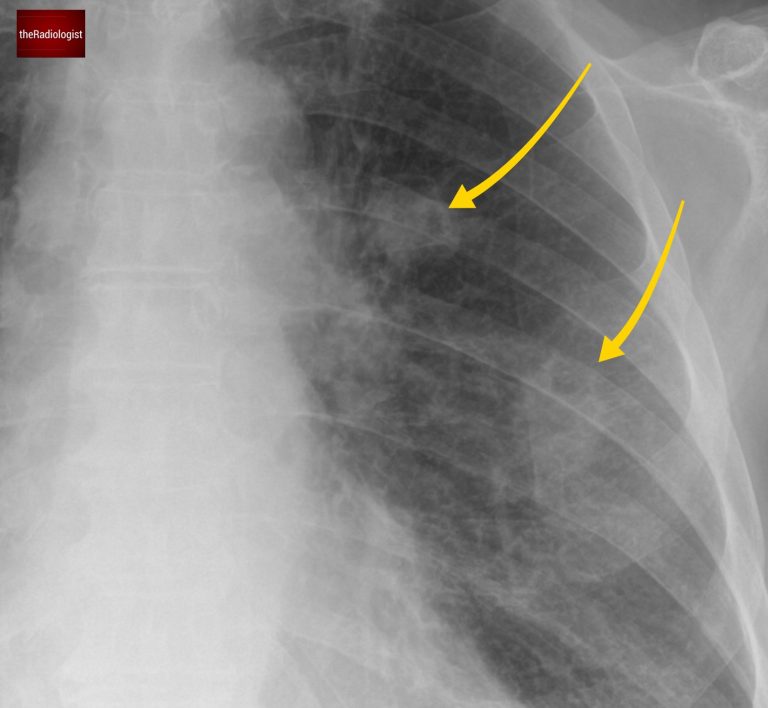
Look closely and you will see multiple lung nodules, some of which show internal lucency, ie cavitation
Single cavitating lesion
The differential for a single cavitating lesion is usually limited:
- Infection, consider Staph Aureus, Klebsiella, fungal infection and tuberculosis (TB).
- Primary lung cancer, classically squamous cell carcinoma.
Multiple cavitating lesions
Now, multiple cavitating lesions, like in this case, expand the differential. I like to use the mnemonic STARE:
| Cause | |
|---|---|
| S | SCC metastases |
| T | TB and atypical infection |
| A | ANCA positive vasculitis |
| R | Rheumatoid nodules |
| E | septic Emboli |
Let’s have a look at each of these in a bit more detail:
SCC metastatic disease
There are several causes of cavitating lung metastases but they most commonly derive from a squamous cell carcinoma, often originating from the lung or head and neck.
TB and atypical infection
Always an important consideration, consider fungal infection such as aspergillosis. With TB look for involvement of the right upper lobe and apical right lower lobe, tree-in-bud nodularity and necrotic lymph nodes.
ANCA-positive vasculitis
Most notably granulomatosis with polyangiitis (GPA), formerly known as Wegener’s granulomatosis.
Screening for ANCA antibodies is typically advised in these cases: I have seen several cases picked up over the years after recommending an ANCA screen.
Rheumatoid nodules
These are usually small and peripheral, some of which can cavitate.
Septic emboli
Also typically small and peripheral. Also look out for wedge shaped opacities – see this case for more on septic emboli.
Assessing the mediastinum
Let’s go back to our case. On closer inspection, the X-ray reveals an abnormal aortopulmonary (AP) window.
- Normally, this area has a concavity, but here it appears full, suggesting mediastinal lymphadenopathy.
- This observation pushes metastatic disease and TB higher up the differential.

Looking at the mediastinum there is filling of the AP window suggesting lymph node enlargement.
CT scan assessment
A post contrast CT scan was performed which confirmed the chest X-Ray findings of multiple cavitating lung lesions, enlarged mediastinal lymph nodes involving the aortopulmonary window as well as a bilateral pleural effusions.
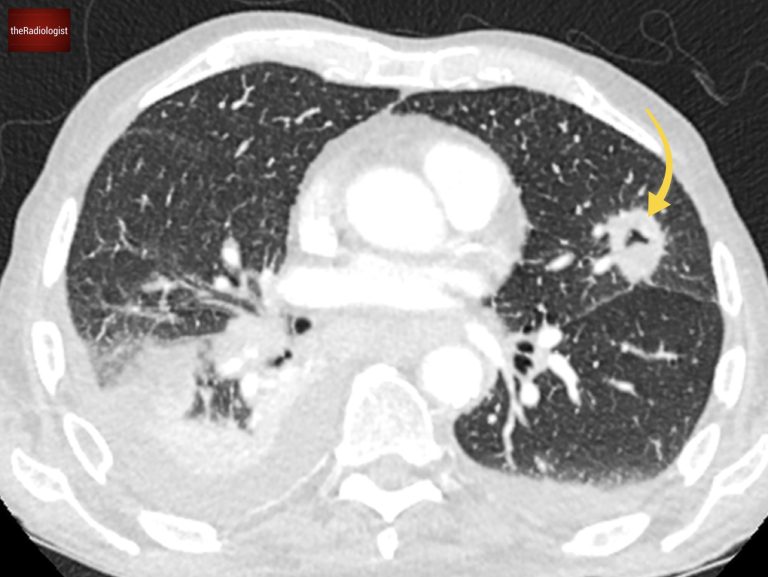
The cavitating lesions are confirmed on CT.
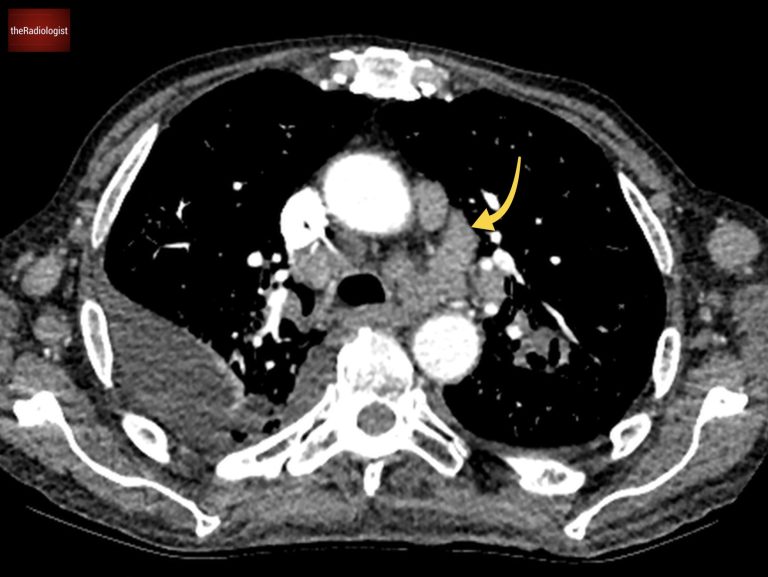
On soft tissue windows we can see a right pleural effusion, left axillary node and enlarged mediastinal nodes. AP window nodes (arrow) are seen accounting for the X-Ray abnormality.
Underlying diagnosis
The diagnosis in this case came from biopsying groin lymph nodes, which revealed a metastatic neuroendocrine tumor.
This isn’t the most common cause of cavitating lung lesions, but it emphasises the need for a tissue diagnosis when imaging findings aren’t conclusive.
KEY POINTS
Use the STARE mnemonic when you see multiple cavitating lesions on X-Ray: this will cover the majority of causes and gives you a systematic approach.