Cavernoma
On CT and MRI head
Introduction
A woman in her 40s presents after a head injury and loss of consciousness. A non-contrast CT is performed, and a high-density lesion is spotted in the occipital lobe. But the underlying diagnosis is not clear.
This case walks you through how to assess an unusual hyperdense lesion on CT, when to suspect something beyond trauma, and how MRI can confirm the diagnosis.
A useful reminder that not every bright spot on a head CT is a bleed.
Case introduction
A female patient in her 40s presented to the emergency department after a head injury. She had lost consciousness earlier the same day and underwent a non-contrast CT scan of her head.
Have a look at the scan below.
I know you want to get going but you may need to wait a few seconds for the scan to load. Tap the first icon on the left to scroll.
Video explanation
Here is a video explanation of this case: click full screen in the bottom right corner to make it big. If you prefer though I go through this in the text explanation below.
CT scan findings
Looking at the CT scan, on first inspection there is a high density focus within the right occipital lobe. Now any high density on an acute CT head warrants suspicion for acute haemorrhage.
On closer inspection the lesion appears heterogeneous with possible flecks of calcification. There is no mass effect so the surrounding structures such as the right lateral ventricle are not distorted. Also there is no oedema (a low density rim would suggest vasogenic oedema).
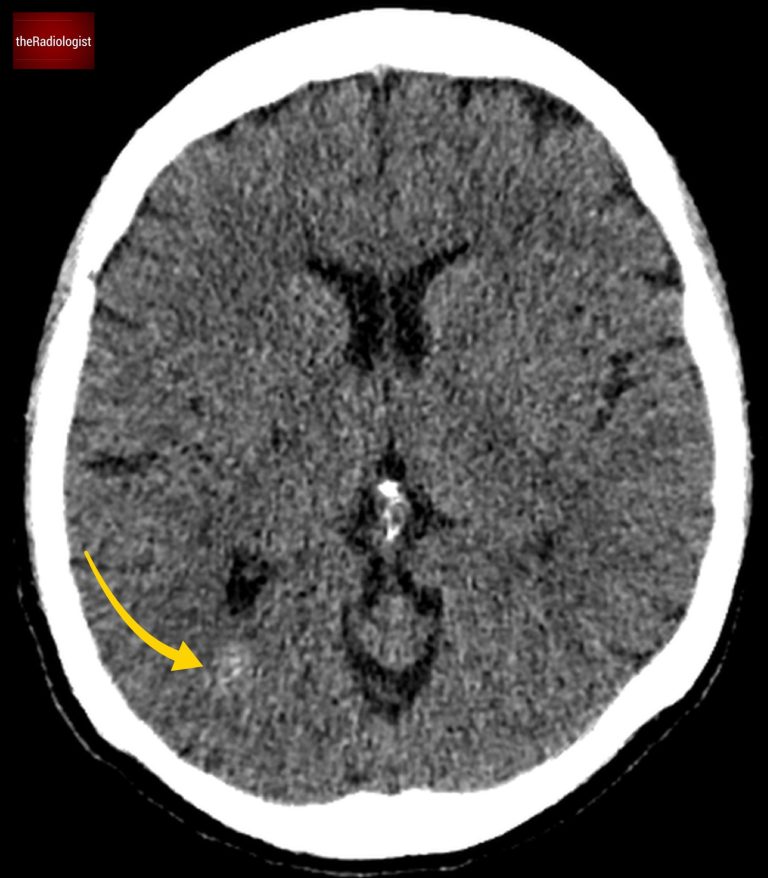
Did you spot the high density lesion within the right occipital lobe?
Comparison with intraparenchymal haemorrhage
Now, let’s compare this to a known case of intraparenchymal haemorrhage:
Firstly the lesion in our case is not as dense as a typical acute haemorrhage.
There’s no surrounding oedema.
The presence of calcification further raises suspicion for something other than trauma-related haemorrhage.
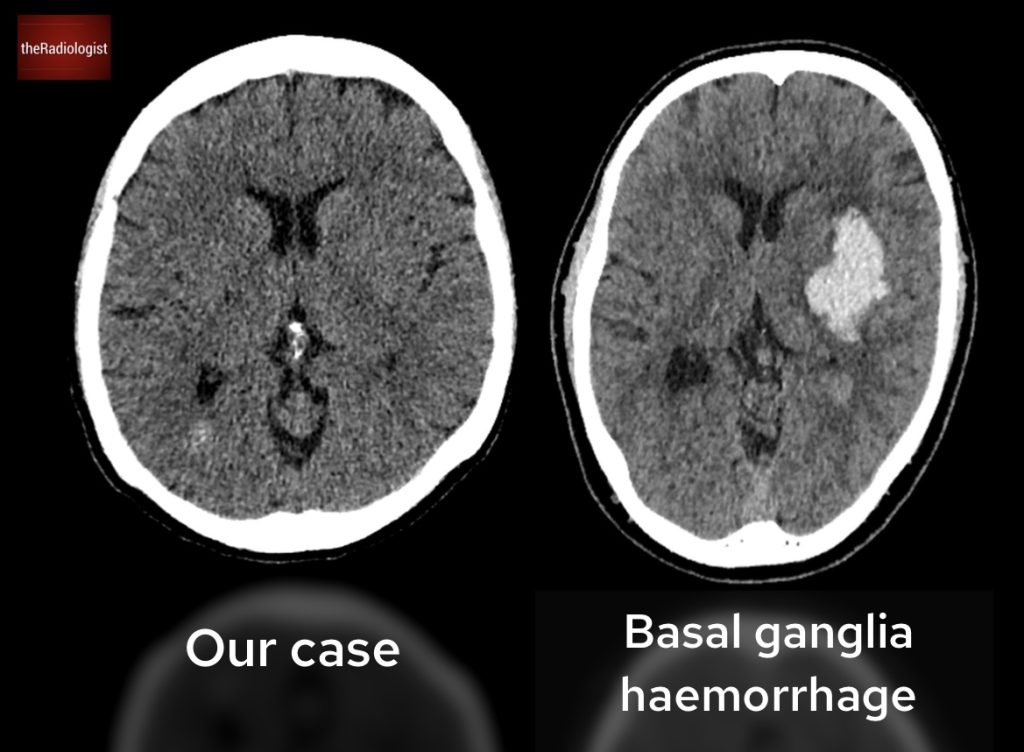
Compare our case (left) with a case of confirmed basal ganglia haemorrhage on the right.
MRI findings
Given the unusual CT appearance, the patient underwent an MRI. Here’s what the MRI revealed:
- T2 Sequence:
- The lesion has a “popcorn” appearance, with a low-intensity rim: a hallmark feature.
- T1 Sequence:
- There’s high signal intensity, indicative of blood products.
- T1 post gadolinium contrast:
- The lesion shows no enhancement, helping us rule out certain neoplastic or inflammatory causes.
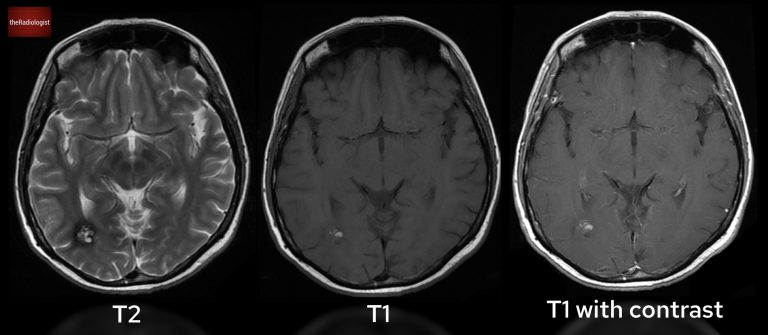
Have a look at T2 (left), T1 (centre) and T1 post gadolinium (right) sequences.
What is a cavernoma?
The imaging findings point to a cavernous malformation (also known as a cavernoma or cerebral cavernous venous malformation).
What Are Cavernous Malformations?
- These are low-flow vascular malformations composed of thin-walled, dilated capillary spaces filled with blood.
- They are found in roughly 1 in 625 patients.
- Unlike haemangiomas, they are not true proliferating neoplasms.
- They can vary in size, shrink, or grow over time. They range in size from under a millimetre to several centimetres.
- They’re often asymptomatic but can bleed, causing neurological deficits or epilepsy.
Treatment
If found incidentally, cavernous malformations are often managed conservatively and monitored.
Surgical resection may be considered in cases of:
- Recurrent haemorrhage.
- New neurological deficits.
- Refractory epilepsy.
KEY POINTS
When evaluating a possible intracerebral bleed on CT that lacks the classic brightness of a cerebral haemorrhage think about a cavernous malformation.
These lesions are best confirmed with MRI, where their characteristic features usually show through.