Bronchiectasis
On chest X-Ray and CT
Introduction
Bronchiectasis is a chronic condition characterized by irreversible dilatation of bronchi. It most commonly presents with an ongoing cough and excess sputum production.
But we care about radiology here so we’re going to look at the imaging findings. Chest X-Ray is often done as a first line in these patients and the findings can be subtle whilst CT is a cornerstone of diagnosis.
In this article we will go through a real life case of bronchiectasis to try and illustrate the radiographic and CT appearances. We will go through the definition of bronchiectasis, its causes and the different types of bronchiectasis we see on CT.
Case introduction
A man in his 20s attends his GP after struggling with recurrent chest infections. A chest X-ray is performed—do you see anything abnormal? This is a tricky one.
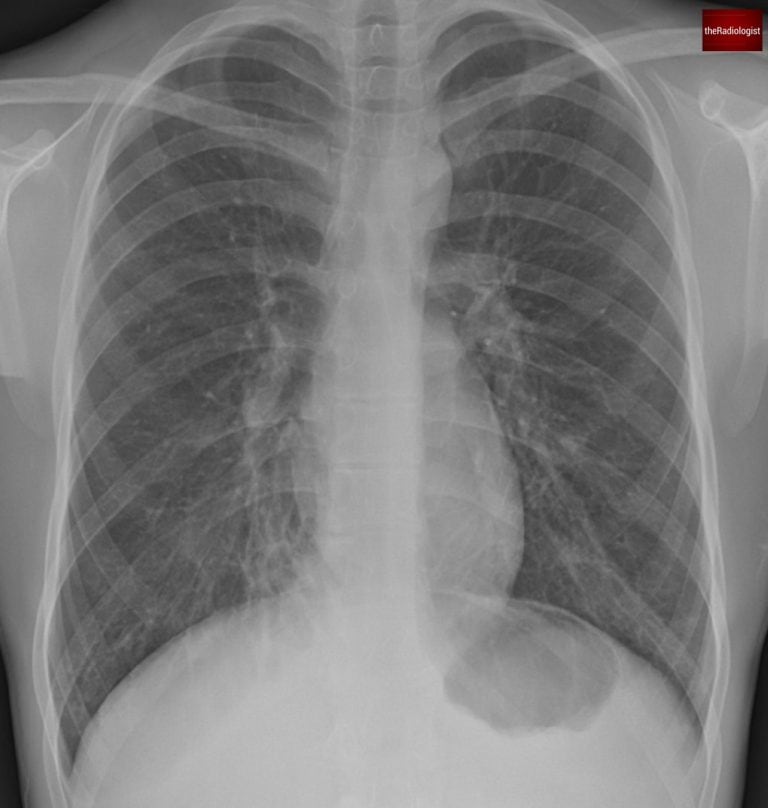
PA view of a chest X-Ray of a male in his 20s
Video explanation
Here is a video explanation of this case: click full screen in the bottom right corner to make it big. If you prefer though I go through this in the text explanation below.
Case findings
When looking at a chest X-ray for someone in their 20s, you generally expect clear lungs with no abnormalities. So even subtle abnormalities in a patient of this age should not be taken lightly.
Let’s start by having a look at the right lung near the right heart border and compare with the same area within the left lower zone.
We can see the area of lung by the right heart border looks abnormal and if you look closely you can just make out a ‘ring shadow’. Ring shadows on a chest X-ray raise the possibility of bronchiectasis.
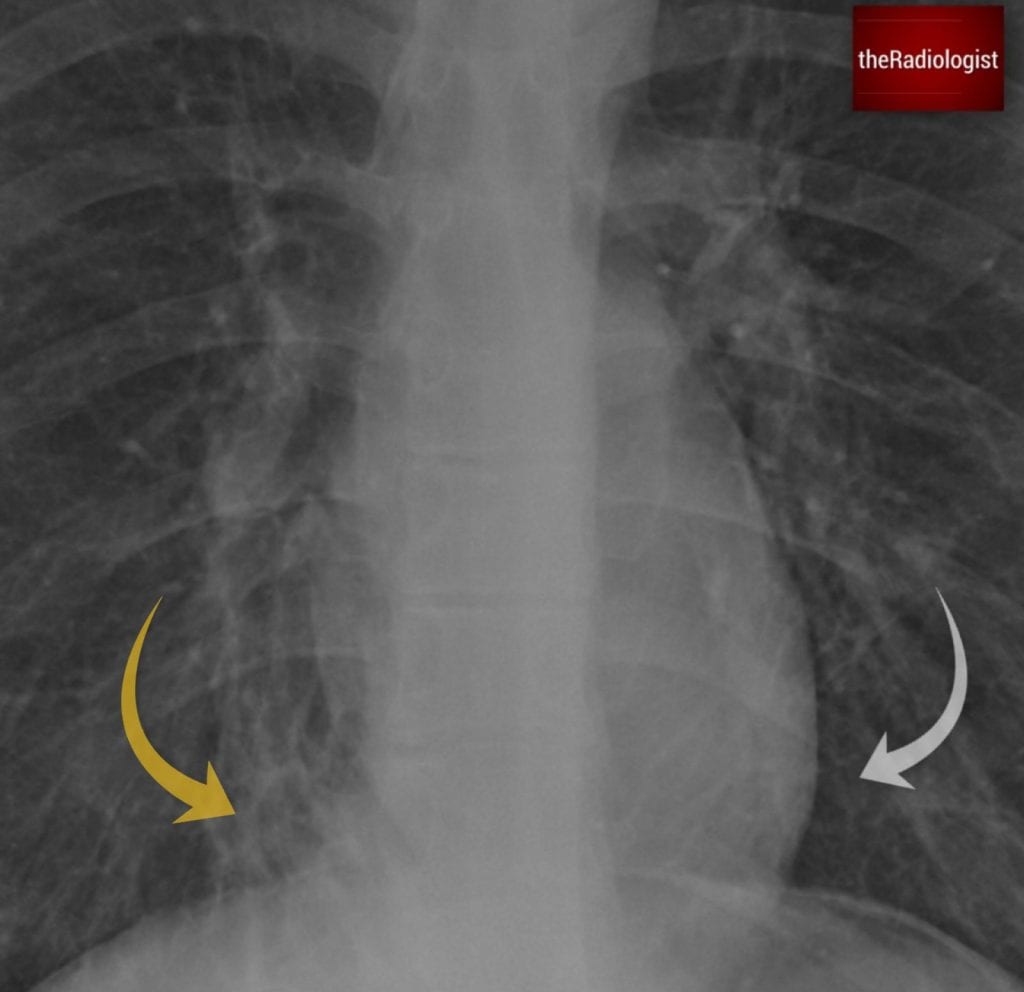
Compare the area of lung adjacent to the right (yellow arrow) and left heart border (white arrow) and you will see the region adjacent to the right heart border appears abnormal. Look closely and you will see a ‘ring shadow’ raising the possibility of bronchiectasis.
Bronchiectasis definition
Bronchiectasis is a condition where the airways become abnormally dilated and damaged. Note the airway changes in bronchiectasis are irreversible.
How do you diagnose bronchiectasis?
A CT scan is the gold standard because it lets us see the airway size and structure more clearly. Normally, the airway should be the same size or smaller than the pulmonary artery running alongside it. In bronchiectasis, the airway is larger than the adjacent pulmonary artery. On CT scans this can give something called a ‘signet ring’ sign.
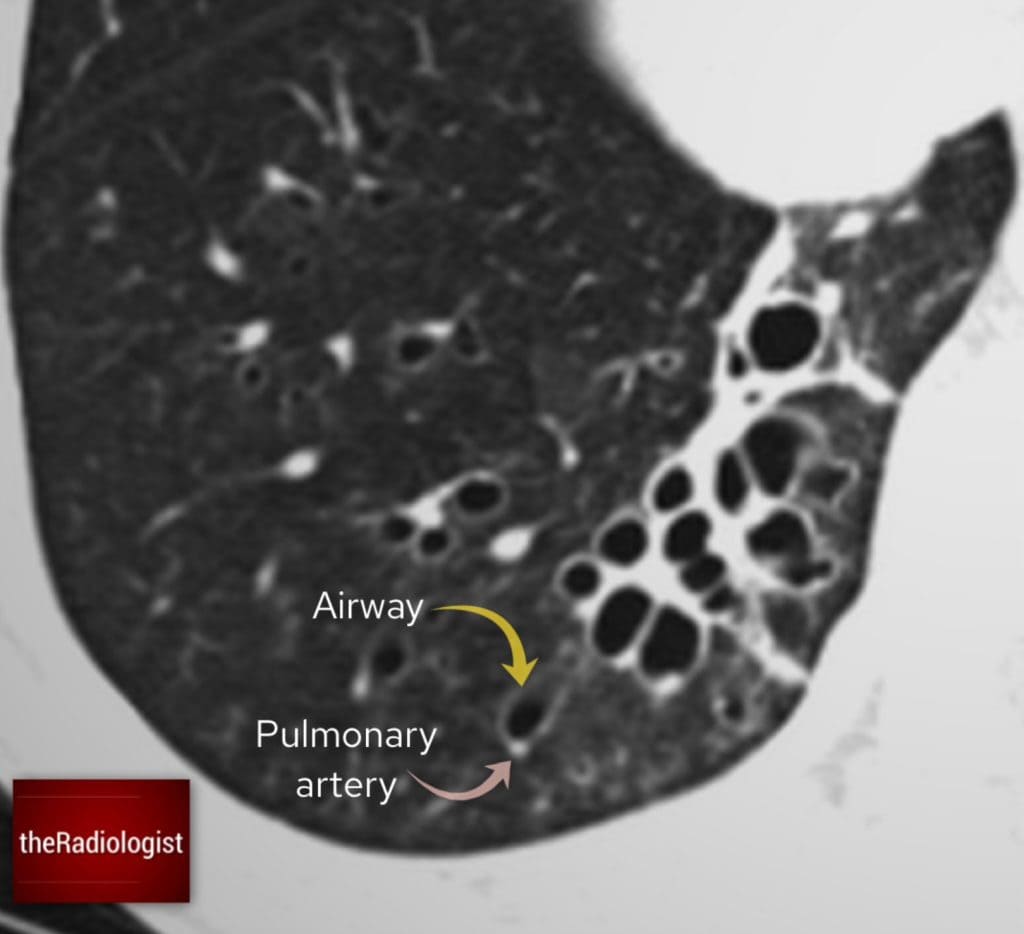
In normal circumstances the airway should be smaller or the same size as the pulmonary artery running beside it. I often think can I fit the pulmonary artery into the airway as if it were a hole – if I can’t then there is no bronchiectasis.
Causes of bronchiectasis
Bronchiectasis can sometimes happen without an obvious cause (idiopathic), but there are several things that can make someone more likely to develop it:
| Cause | Notes |
|---|---|
| Recurrent infection or serious childhood infection | Severe or repeated chest infections, especially in childhood, can damage the airways permanently. Illnesses like whooping cough or measles can lead to long-term lung damage. |
| Cystic fibrosis | This condition leads to thick mucus buildup, causing chronic infections and, ultimately, bronchiectasis. If you see bronchiectasis on a CT scan look for fatty replacement of the pancreas and this can lead you to a diagnosis of cystic fibrosis. |
| Allergic bronchopulmonary aspergillosis (ABPA) | A hypersensitivity reaction to the fungus Aspergillus, almost exclusively seen in asthmatics, causes central bronchiectasis and mucus-filled bronchi that can look like a finger-in-glove sign on CT. High-density mucus on CT? That’s a big clue that ABPA is the underlying cause. |
| Airway obstruction | If something is blocking an airway (like a tumour or foreign body), mucus builds up behind it, leading to localised bronchiectasis so look proximal to the bronchiectasis if focal on CT to see if anything is blocking the airway. |
| Other | Other causes include primary ciliary dyskinesia, immunodeficiency disorders and rheumatoid arthritis. |
Case workup
On the CT scan if we assess the right lower lobe we will see dilatation of the airways and bronchiectasis.
We can also see signs of airway inflammation:
- Bronchial wall thickening – A sign of ongoing airway inflammation.
- Groundglass centrilobular nodules – These suggest inflammation affecting the small airways, possibly infection in the context of bronchiectasis.
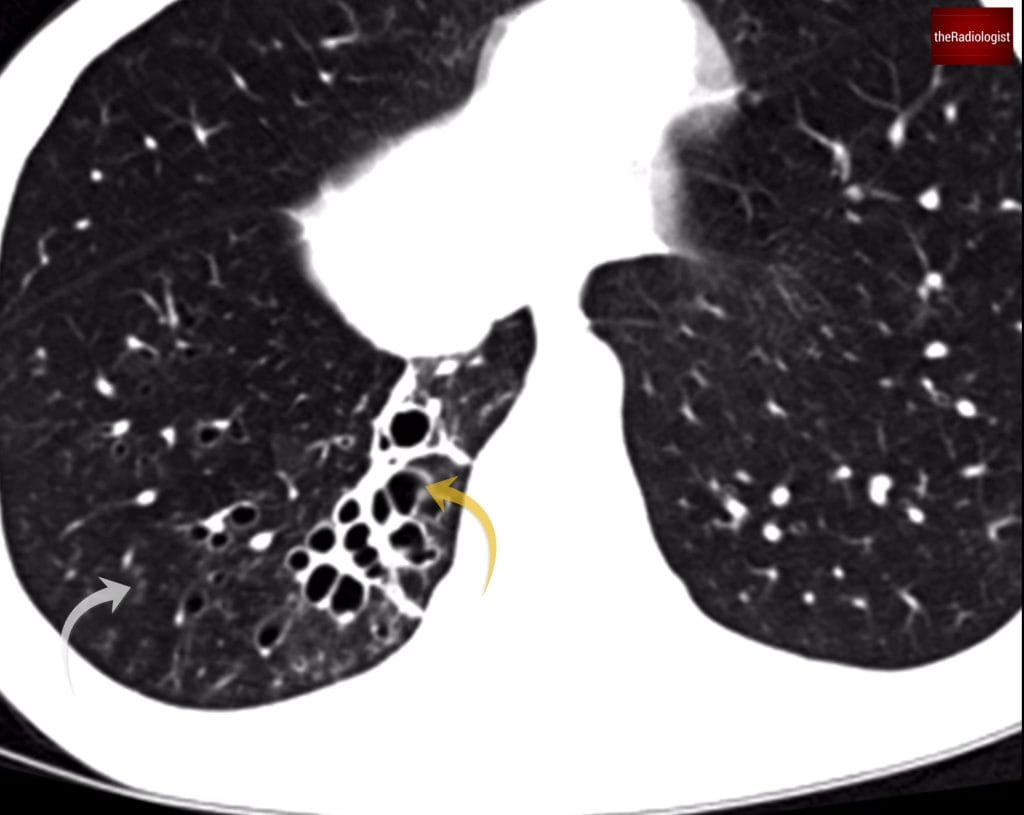
Within the posterior segment of the right lower lobe there is clear bronchiectasis (yellow arrow) and signs of airway inflammation. The grey arrow points at centrilobular ground nodules, a sign of small airway inflammation.
Types of bronchiectasis
We can describe bronchiectasis in different ways when we see it on CT. We can think of it as a spectrum.
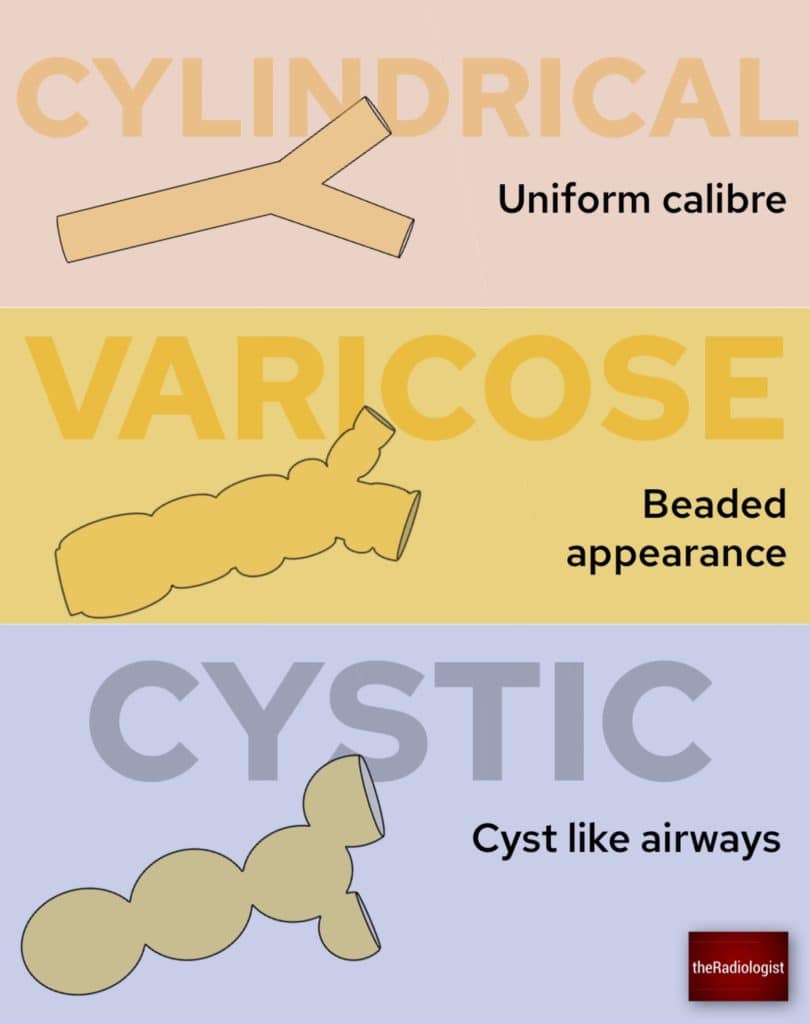
We can think of bronchiectasis as a spectrum of cylindrical, varicose and cystic bronchiectasis.
Cylindrical bronchiectasis
Airway walls look smooth and tubular. Ie they look like cylinders.
Varicose bronchiectasis
The airways look beaded, like a string of pearls.
Cystic bronchiectasis
The most severe form, where airways look like clusters of cysts, sometimes described as a ‘bunch of grapes’ and this is what we can see in our case. Cystic bronchiectasis can mimic cystic lung disease or honeycombing as seen in lung fibrosis.
How can we tell the difference? with cystic bronchiectasis the cysts will follow the course of the airways and you should be able to trace the cysts back to the proximal airway.
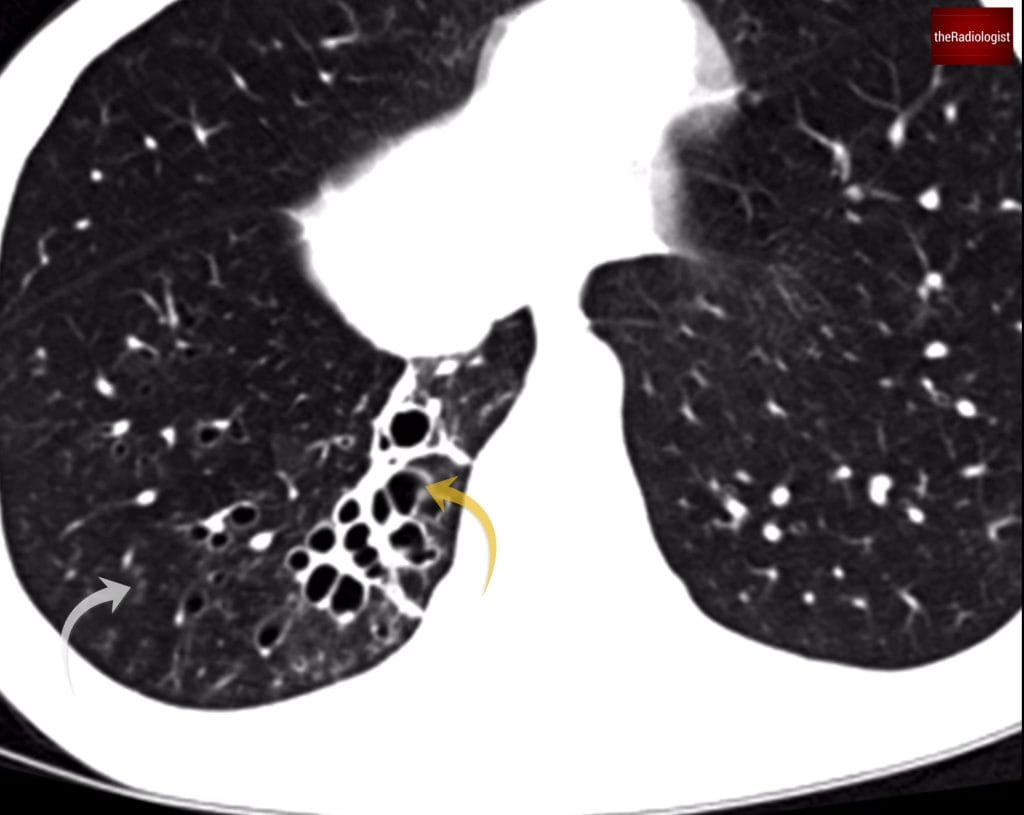
Cystic bronchiectasis is thought to resemble a ‘bunch of grapes’.
Reflection
Now that we’ve analysed the CT, let’s go back to the original chest X-ray. The ring shadows represented dilated airways seen end-on and are something to look out for on X-Ray.
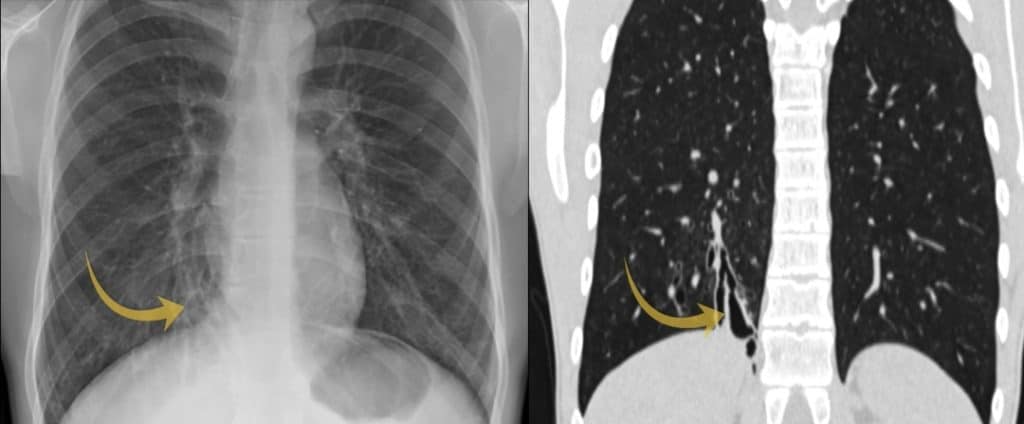
The area of abnormality on the chest X-Ray correlates with the area of cystic bronchiectasis seen on CT.
KEY POINTS
X-Rays in young patients in particular should be ‘clean’ – if you see an abnormality you need to be able to explain it.
Ring shadows may represent underlying bronchiectasis for which CT is the gold standard for diagnosis.