Pelvic X-Ray Guide
How to interpret pelvic X-Rays
Introduction
CT is the gold standard for characterising fractures and guiding surgical planning, but the AP pelvic X-ray remains the initial imaging test in many emergency settings worldwide. Interpreting this film can be challenging but with a structured review system, you’ll be able to pick up important injuries quickly.
General pelvic anatomy
The pelvis is a ring-shaped structure composed of the two innominate bones (each formed by the ilium, ischium, and pubis), the sacrum, and the coccyx. It provides stability and weight transfer between the axial skeleton and lower limbs, protects pelvic organs, and serves as a major site of muscle and ligament attachment.
Bony structures
- Ilium: The broad, wing-shaped portion forming the superior pelvis. The iliac crests are palpable landmarks, while the anterior superior iliac spines (ASIS) and posterior superior iliac spines (PSIS) are key reference points.
- Ischium: Forms the posteroinferior part of the pelvis, including the ischial tuberosities: the major weight-bearing points when sitting.
- Pubis: The anterior part of the pelvis, with left and right pubic bones joining at the pubic symphysis.
- Acetabulum: A deep, cup-shaped socket formed where the ilium, ischium, and pubis meet. It articulates with the femoral head to form the hip joint.
- Sacrum and coccyx: Form the posterior midline of the pelvis and articulate with the ilia at the sacroiliac joints.
On plain radiographs, the integrity of the pelvic ring, symmetry of obturator foramina, width of the pubic symphysis, and cortical outlines of the iliac wings, acetabula, and sacroiliac joints should all be traced. CT offers superior sensitivity for fractures, especially of the sacrum and acetabula, while MRI provides further evaluation of marrow, cartilage, and soft tissue structures.
Joints and articulations
The pelvis contains three major joints:
- Pubic symphysis: A fibrocartilaginous joint uniting the two pubic bones. It is normally <5 mm wide in adults; widening suggests trauma or diastasis. This is best assessed on AP radiographs and CT.
- Sacroiliac joints: Complex synovial and syndesmotic joints between the sacrum and ilia. They are important load-bearing articulations, and on radiographs and CT they appear as irregular, interlocking joint lines. MRI is superior for early detection of sacroiliitis.
- Hip joints: Ball-and-socket joints formed by the acetabula and femoral heads. Cartilage, labrum, and intra-articular pathology are best seen with MRI, while fractures and alignment are seen well on plain films and CT.
Ligaments
The pelvis is stabilised by some of the strongest ligaments in the body:
- Sacrospinous and sacrotuberous ligaments: Convert the sciatic notches into the greater and lesser sciatic foramina. They are not directly seen on X-ray but may be inferred by altered pelvic ring alignment; MRI can visualise tears or oedema.
- Iliolumbar ligaments: Connect L5 to the iliac crest, stabilising the lumbosacral junction. MRI best demonstrates their integrity.
- Ligaments of the pubic symphysis: Reinforce the symphysis; disruption here suggests unstable pelvic injury.
Neurovascular structures
The pelvis transmits major neurovascular bundles:
- Sacral plexus and sciatic nerves: Emerge through the greater sciatic foramen. On MRI, nerves appear as intermediate-signal bundles, while CT is limited for neural evaluation.
- Obturator nerves and vessels: Pass through the obturator foramina; obturator canal fractures may compress them.
- Iliac vessels: Run along the pelvic brim; seen as soft tissue densities on CT, or flow voids on MRI. Vascular injury is better assessed with CT angiography.
Pelvic X-Ray AP view review areas
The AP view is the primary radiograph for assessing the pelvis. It gives a broad overview of the pelvic ring, acetabula, hips, and proximal femora. While CT is far more sensitive for detecting fractures and defining complex injuries, the AP pelvic X-ray remains the initial investigation in many trauma settings.
Let’s go through a review system: start by screening the soft tissues for any swelling or gas locules before using a mnemonic: PANAP’S RING.
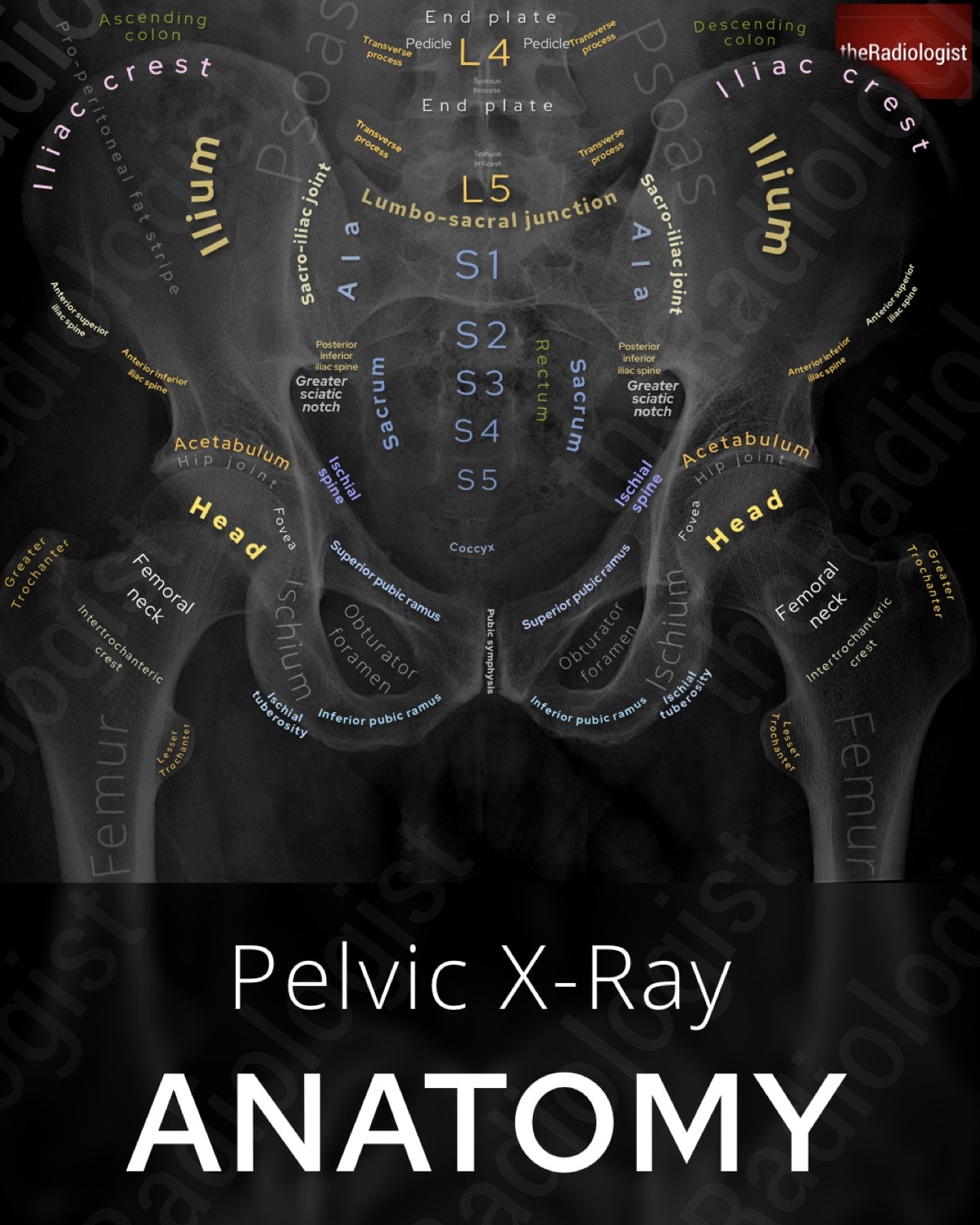
Annotated view of a pelvic X-Ray (AP view)
P: Pubic rami
Trace both superior and inferior pubic rami carefully. These are common fracture sites, especially in low-energy trauma in older patients. Fractures may appear only as faint cortical breaks or irregularities, so look carefully. Always compare both sides for symmetry, and remember: a break in one part of the ring usually means there is a second injury elsewhere.
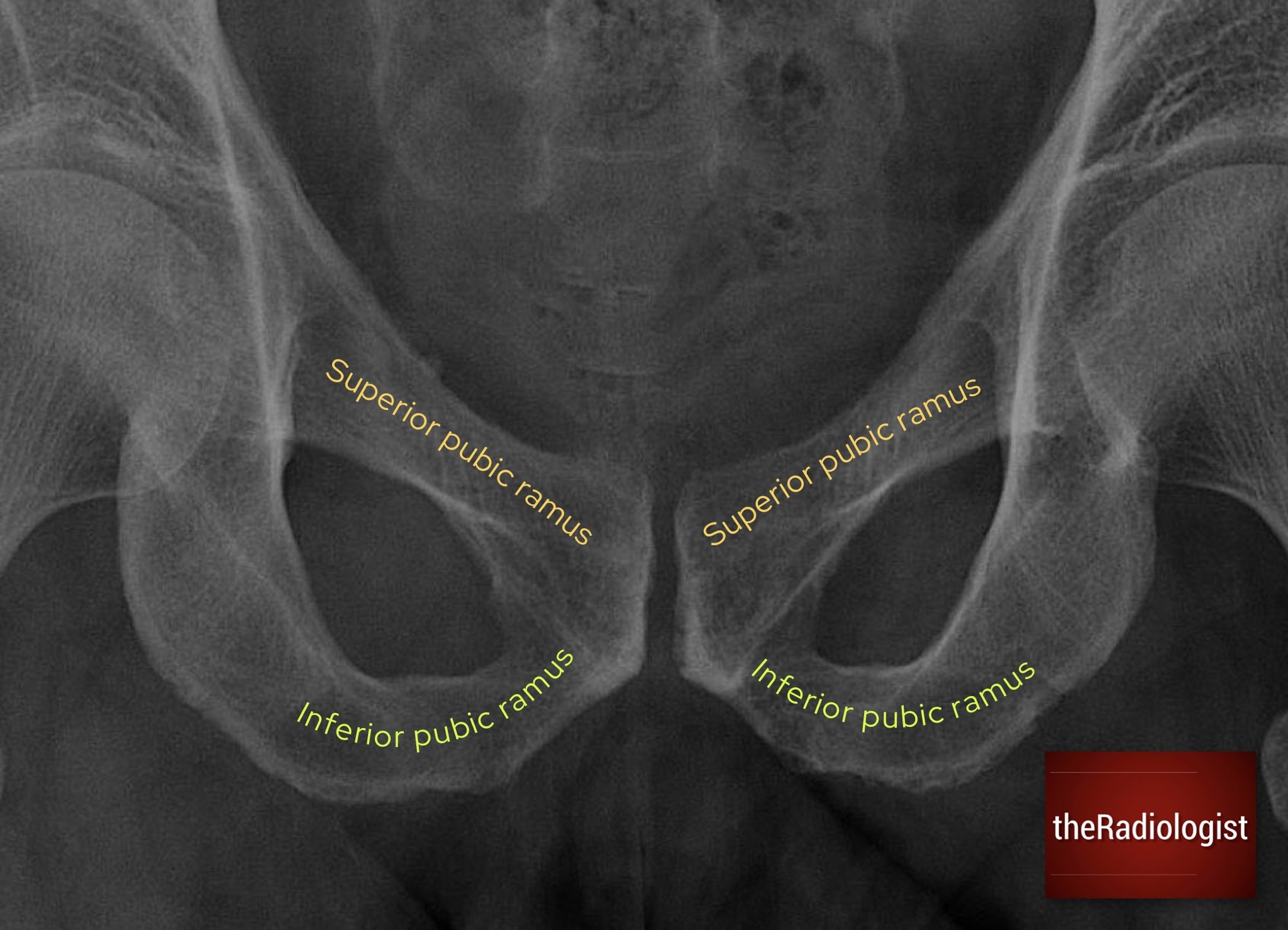
Pay close attention to both the superior and inferior pubic rami looking for any subtle fractures.
On this film if you follow the cortex of the left sided inferior pubic ramus you will see a break in the cortex and a fracture line.
A: Acetabulum
An acetabular fracture can be tricky to pick up so following these three lines can help pick one up:
- Acetabular roof (weight-bearing dome): Look for any step, depression, or sclerosis. Even small changes can affect hip stability.
- Iliopectineal line: Runs from the iliac wing down the pelvic brim to the pubic symphysis, representing the anterior column. Interruption suggests anterior column or wall fracture.
- Ilioischial line: Extends from the sacroiliac joint to the ischial tuberosity, representing the posterior column. Disruption here suggests a posterior column injury.
Any break in these lines, cortical irregularity, or asymmetry should raise concern for acetabular fracture. Subtle displacement may distort the obturator foramen shape. CT is the modality of choice for characterising acetabular fractures, but recognising these classic lines on an AP X-ray can pick up an acetabular fracture.
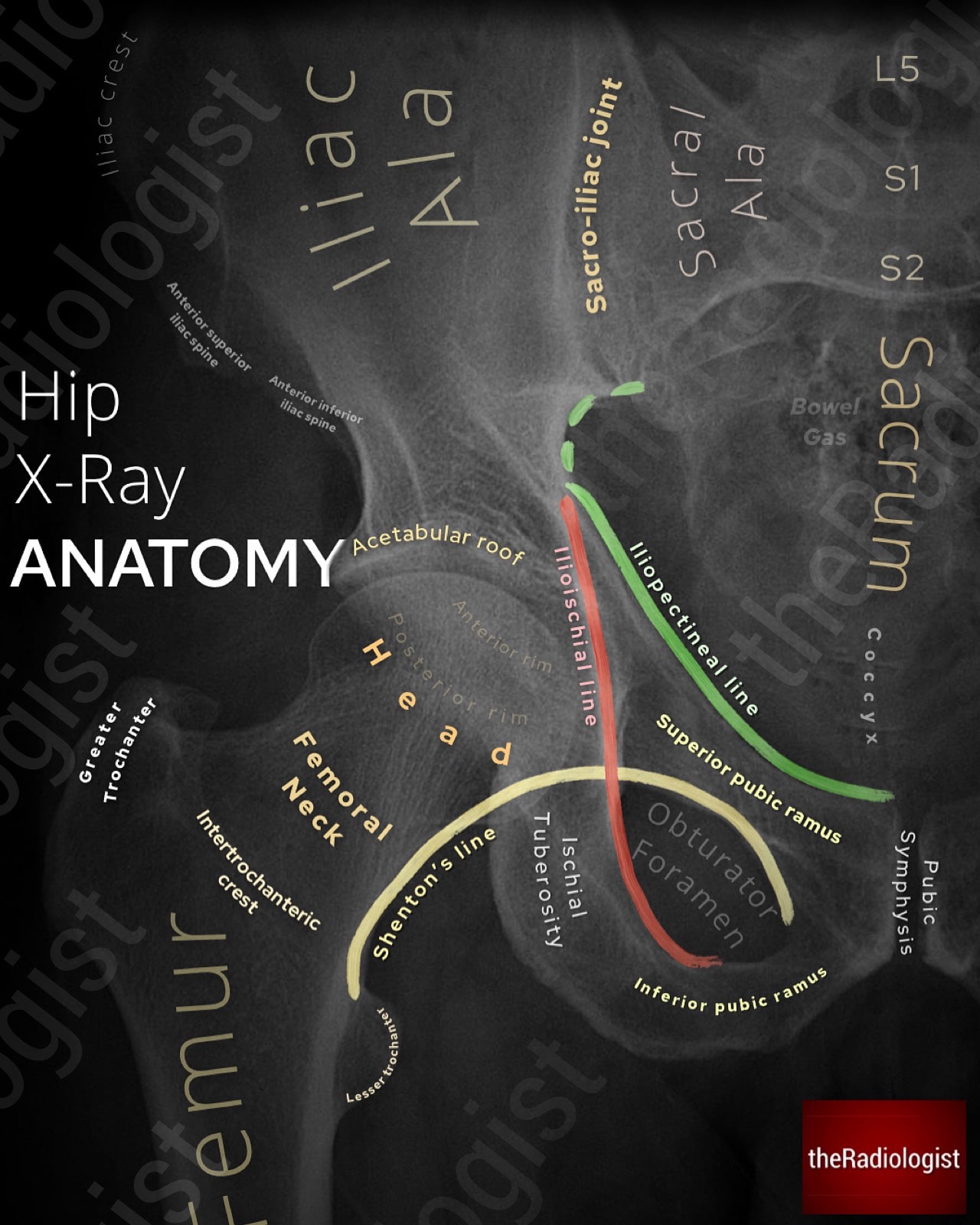
Annotated view of a hip X-Ray showing the acetabular roof, ilioischial line and iliopectineal line
KEY POINT
In the context of trauma:
An abnormal iliopectineal line suggests an anterior column acetabular fracture.
An abnormal ilioischial line suggests a posterior column acetabular fracture.
N: Neck of femur
Examine both femoral necks carefully. Fractures here can be subtle and seen only as a faint lucent line or the internal trabeculae being slightly angled. The line can be sclerotic if there is overlapping bone and an impacted fracture.
Use Shenton’s line, the smooth arc formed by the inferior border of the superior pubic ramus and the inferomedial femoral neck (see the hip X-Ray anatomy diagram above). Any disruption of this in the context of trauma could represent a neck of femur fracture. Also inspect the greater and lesser trochanters for cortical breaks or avulsions.
If you see a neck of femur fracture try and be descriptive as this can guide management. Here are some terms you can use:
Intracapsular fracture: A fracture involving the femoral neck, proximal to the insertion of the capsule. These are at high risk of avascular necrosis and non-union.
Subcapital fracture: A specific intracapsular fracture occurring just below the femoral head.
Transcervical fracture: Runs across the mid-portion of the femoral neck, still within the capsule.
Basicervical fracture: At the base of the femoral neck, bordering the intertrochanteric region.
Intertrochanteric fracture: An extracapsular fracture line running between the greater and lesser trochanters.
Subtrochanteric fracture: A fracture within 5 cm below the lesser trochanter, involving the proximal femoral shaft.
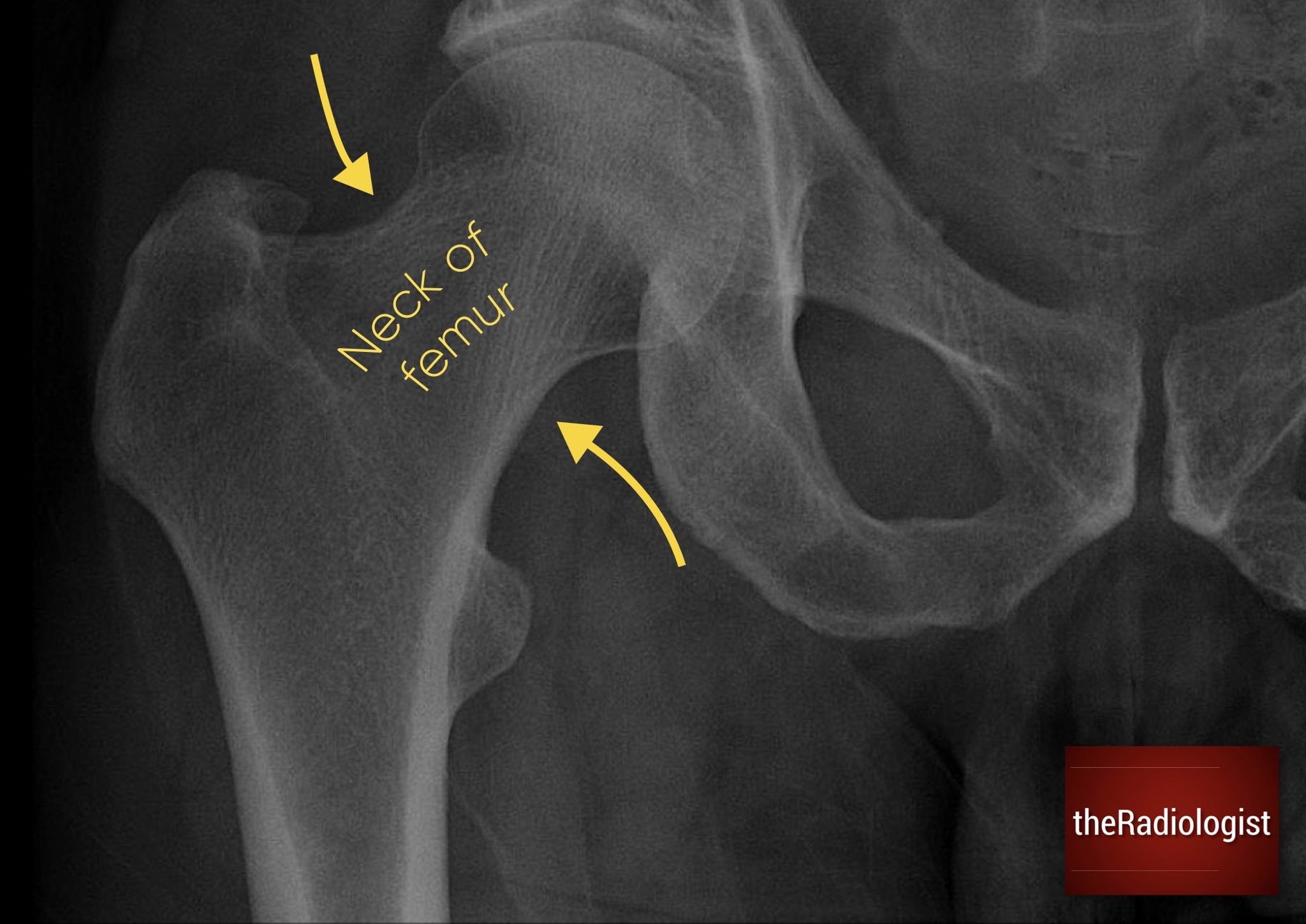
Assess the neck of femur carefully – I always make sure to zoom up as to not miss a subtle break in the cortex or trabecular angulation.
A: Avulsion sites
Avulsion fractures occur when a tendon or ligament pulls off a fragment of bone. Remember a tendon connects muscle to bone and a ligament connects bone to bone.
Knowing muscle and ligament attachment sites helps predict where avulsions may occur. So when assessing areas like the greater or lesser trochanter, look carefully for small bony fragments that could represent avulsion fractures.
Remember there is also a difference between an origin and an insertion. An origin is fixed during contraction whilst an insertion moves during contraction.
Key attachment sites to check:
Iliac crest → abdominal muscles (insert).
ASIS → sartorius (origin).
AIIS → rectus femoris (origin).
Greater trochanter → gluteus medius/minimus, piriformis, obturator internus, gemelli (insert).
Lesser trochanter → iliopsoas (insert).
Ischial tuberosity → hamstrings and adductor magnus (origin).
Pubic symphysis/crest → adductor longus/brevis, rectus abdominis (origin).
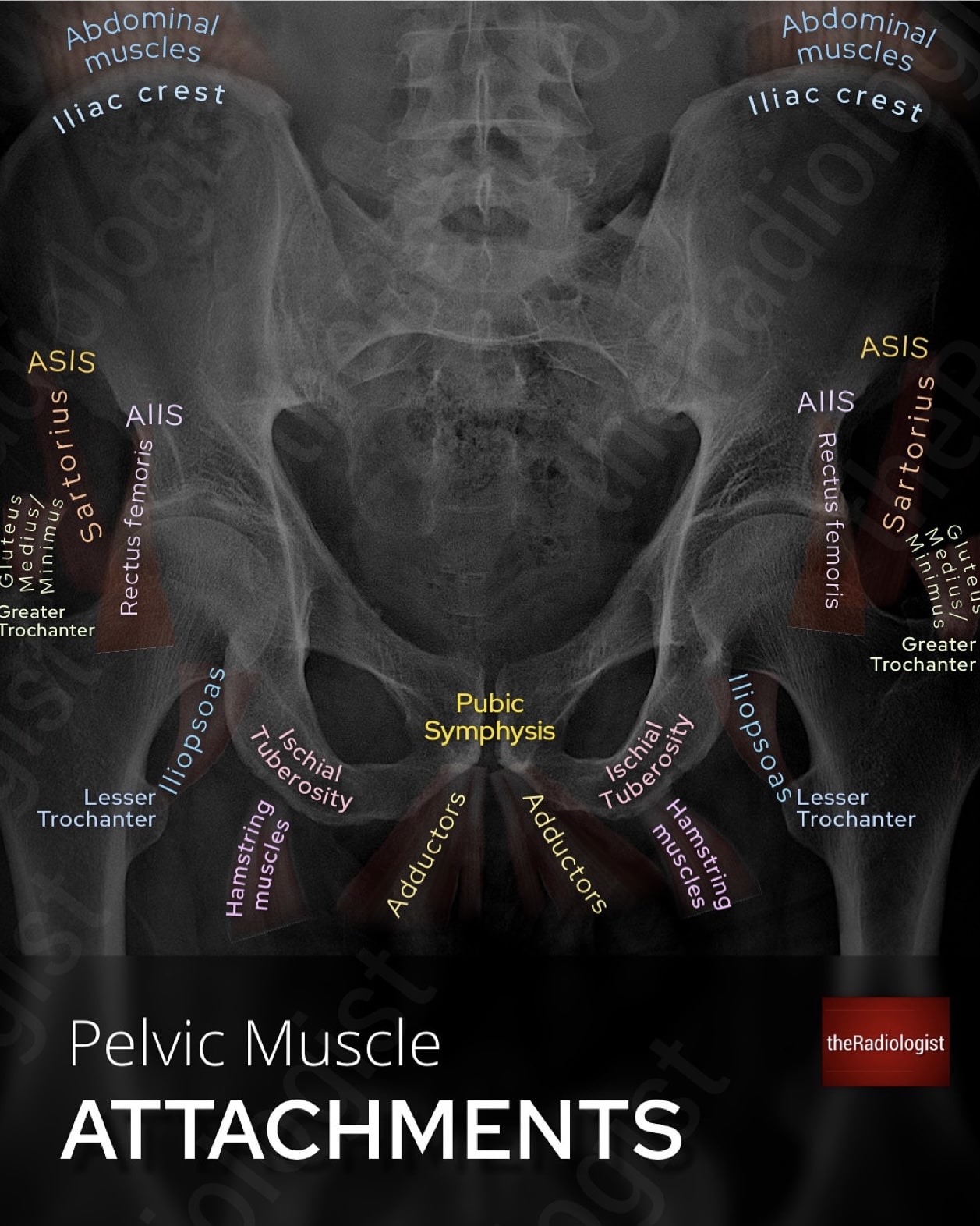
Annotated diagram of a pelvic X-Ray showing pelvic muscle attachments.
P: Pedicles and lumbar spine
The upper part of the AP pelvic film often captures the lower lumbar vertebrae. Always review these for cortical disruption, lytic lesions, or incidental fractures. Don’t miss pathology here just because the film was done for the pelvis. Remember a missing pedicle (’winking owl sign’) could represent an aggressive lesion.
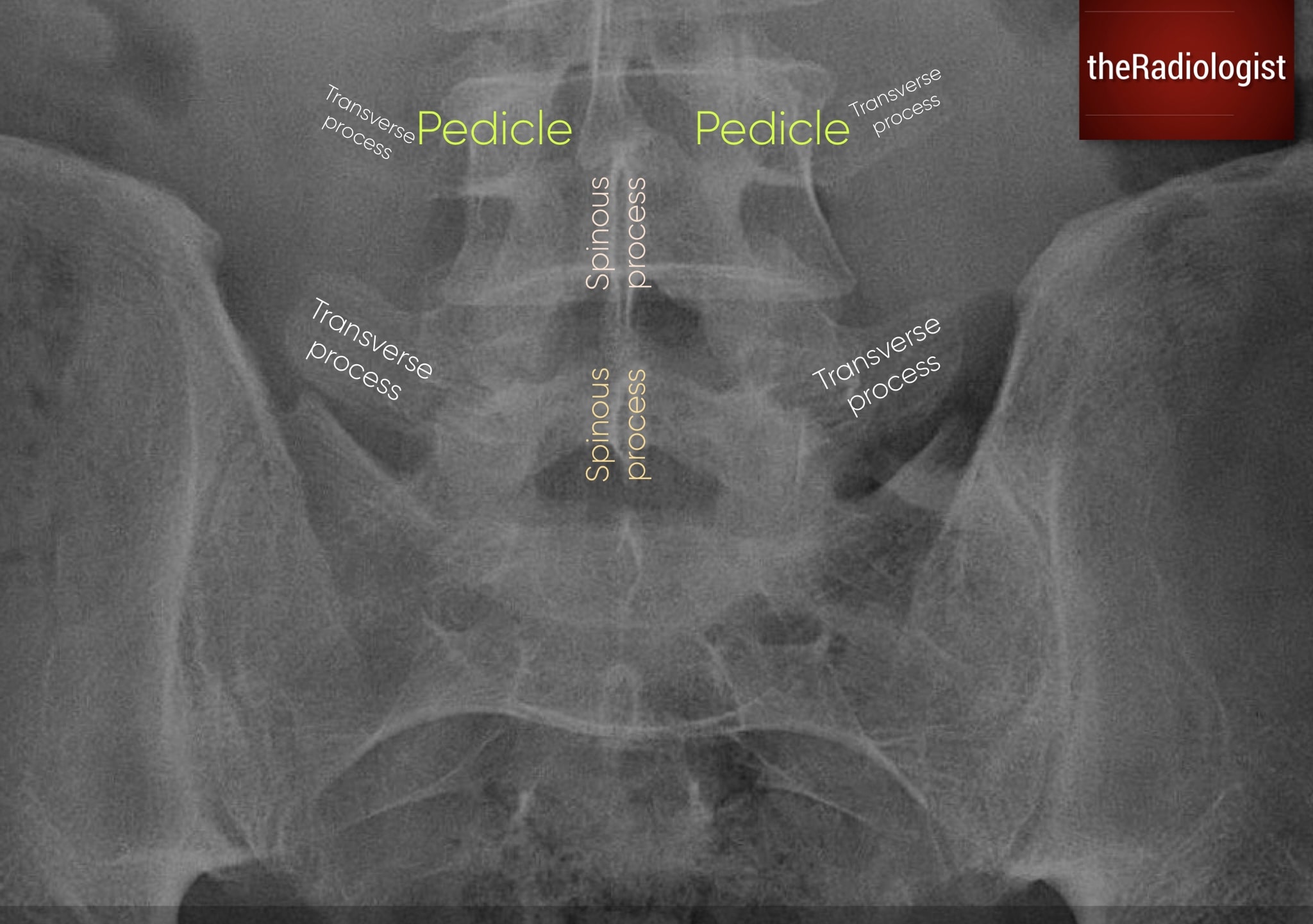
Don’t forget to check the vertebrae and posterior elements within the lower lumbar spine.
KEY POINT
Don’t miss a lumbar spine fracture or lesion on a pelvic X-Ray!
A missing pedicle can mean an aggressive lesion (‘winking owl sign’).
S: Sacroiliac joints
Inspect both sacroiliac joints for symmetry. Widening or displacement can indicate acute trauma although this is not as common as chronic changes. Chronic bilateral sclerosis or ankylosis can be seen in osteoarthritis and seronegative spondyloarthropathies. MRI is best for early inflammatory change, but on plain film we can see more advanced changes.
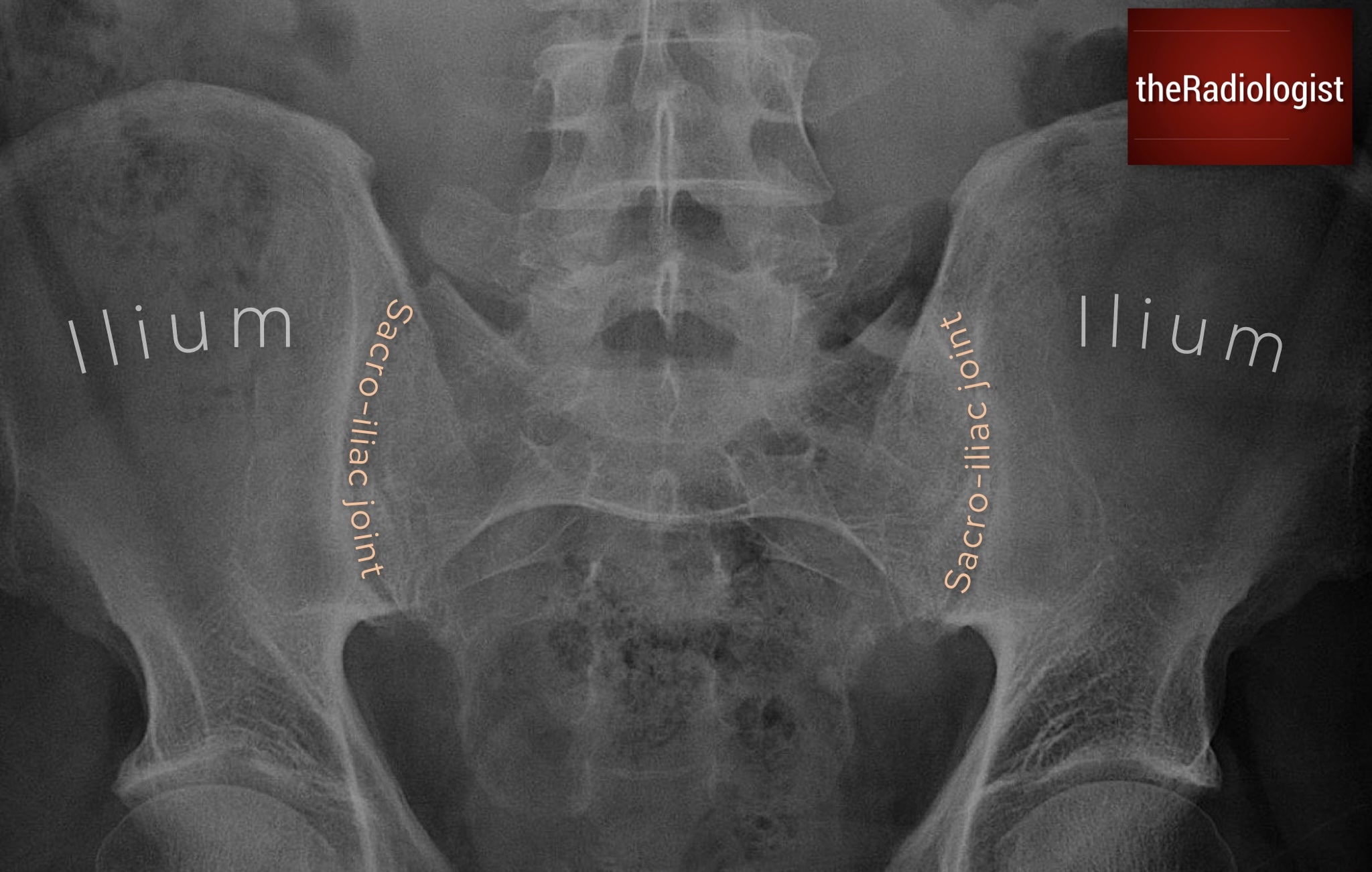
Check the sacro-iliac joints checking for widening, narrowing, ankylosis or sclerosis.
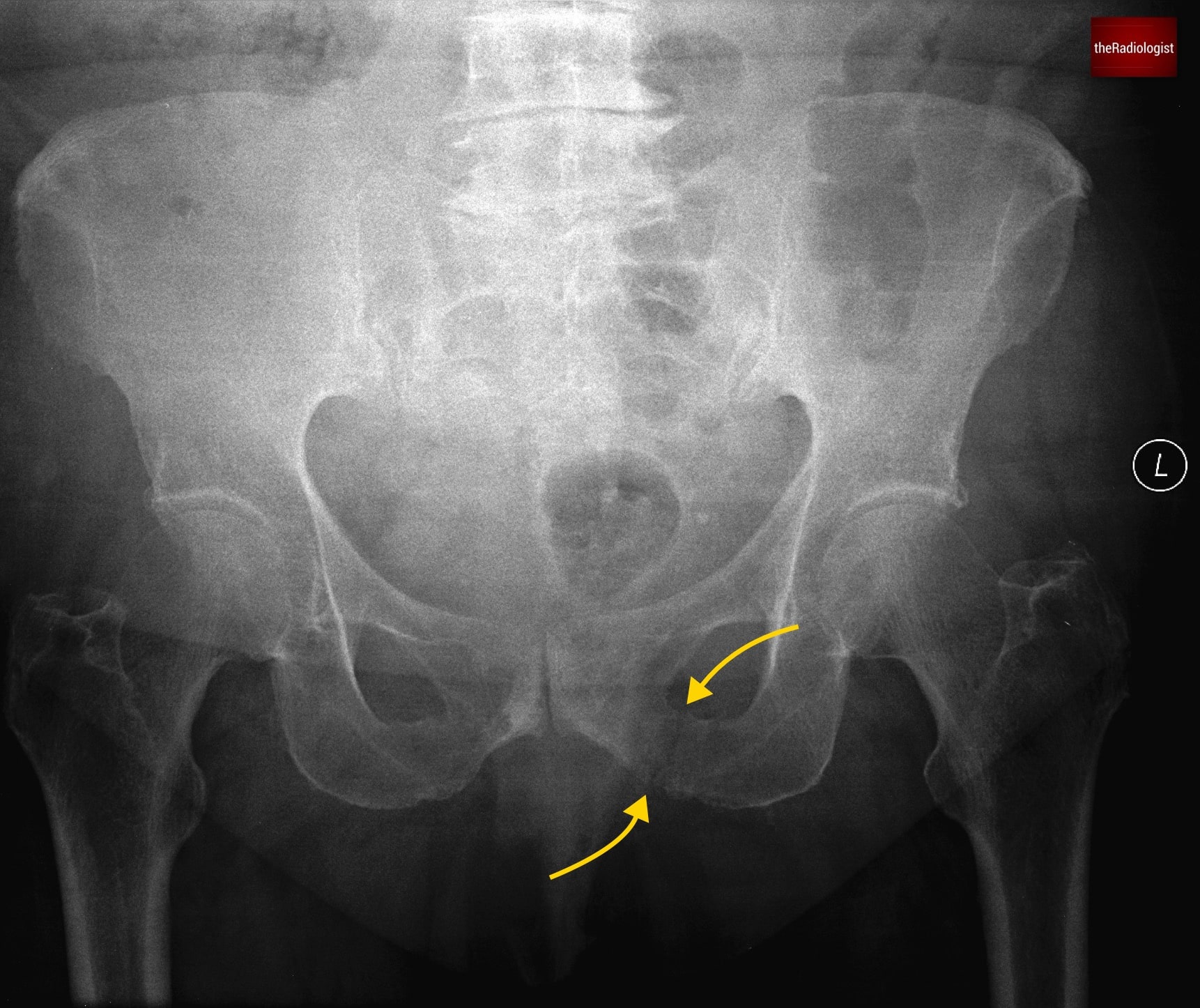
RING: Pelvic ring and obturator foramina
Now check all the rings you can see. Finally, trace the entire pelvic ring looking for a break. In addition both foramina should appear symmetric. Remember: the pelvis acts like a ring: if one break is present, look for another.
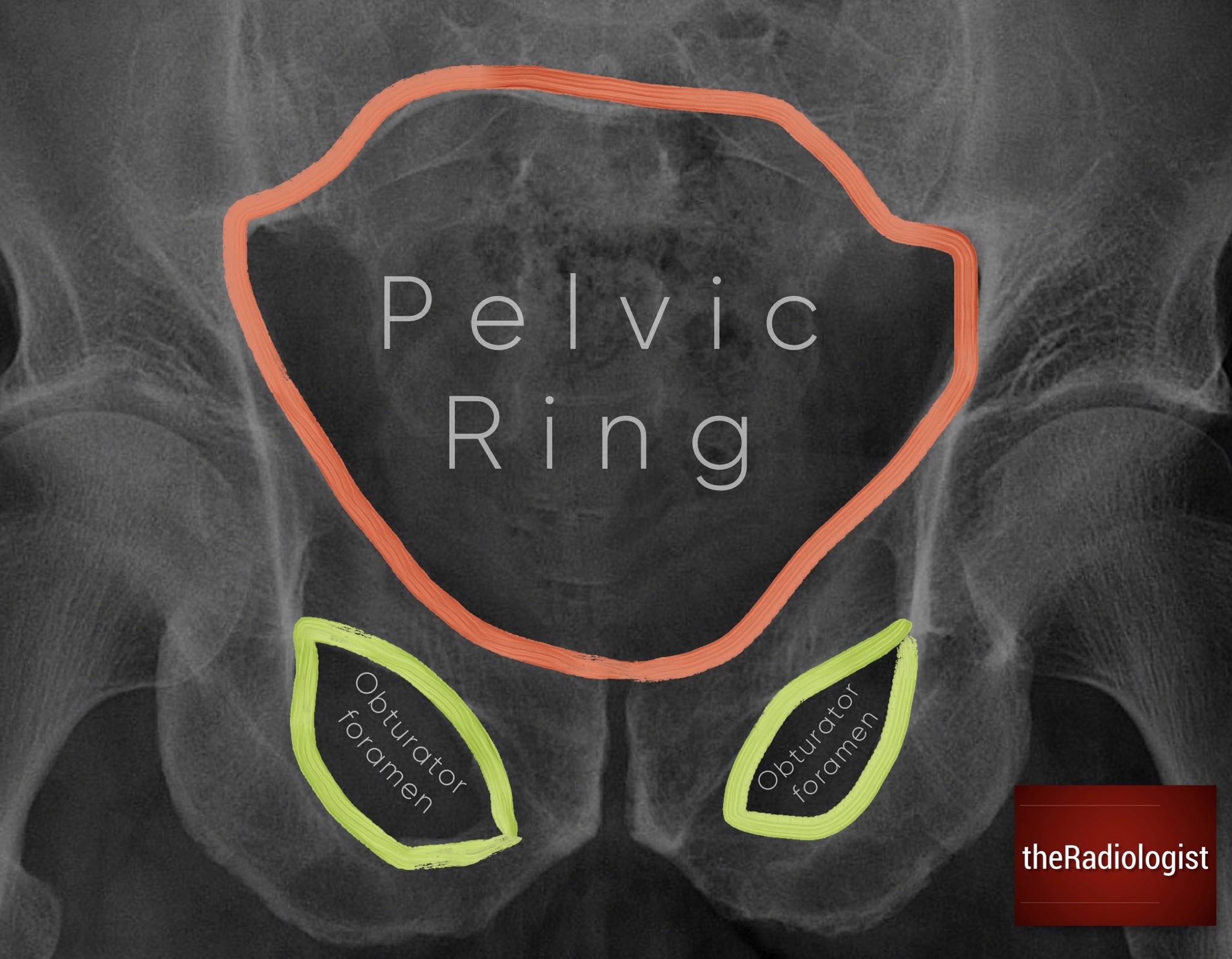
Follow the main pelvic ring and the obturator foramina looking for a break that could mean a fracture.
Final review
After completing each point in PANAP’S RING, zoom out, make the film small and compare sides looking for a bone lesion and any fracture you may not have seen.
Lateral hip X-Ray review
The lateral hip X-ray can be a challenging film to interpret. In some centres it is routinely performed as a supplement to the AP pelvis view, with the aim of excluding a hip fracture. However, no plain film is completely sensitive.
In the UK, NICE guidelines advise proceeding to MRI (or CT if MRI is unavailable within 24 hours) when the X-ray is normal but clinical suspicion remains high. With that in mind, the lateral hip view can still provide useful information when approached in a structured way.
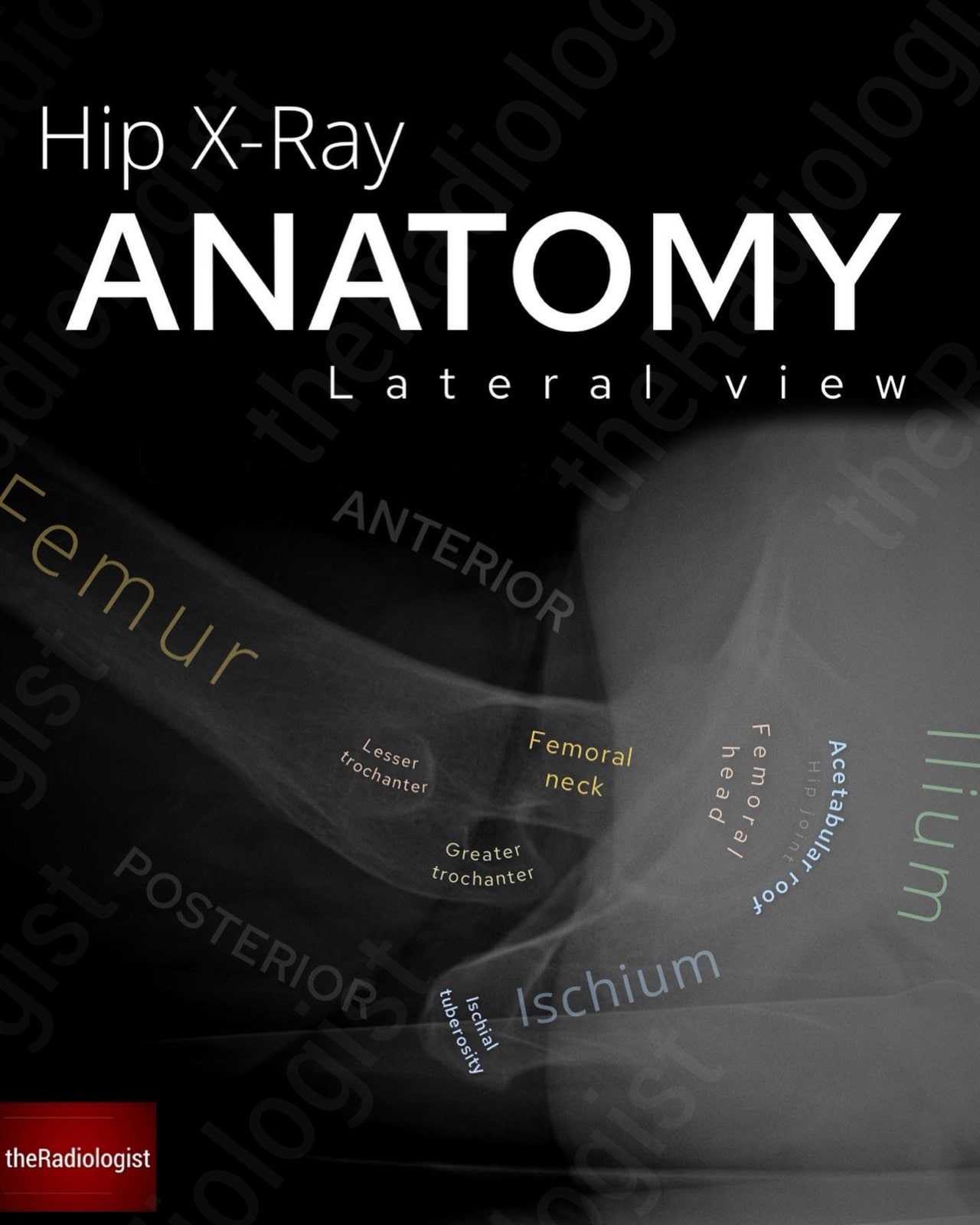
Annotated image of a lateral hip X-Ray.
1. Femoral neck
The femoral neck should be your first focus. Look carefully for a lucent line or cortical disruption, both of which may indicate a fracture. Be aware, though, that impacted fractures can appear as a sclerotic band rather than lucent, as overlapping bones create increased density.
2. Femoral head and acetabulum
Next, assess the articulation between the femoral head and acetabulum and make sure there is no subluxation or dislocation. Trace the outline of the acetabulum wherever it is visible and check for breaks in the cortex.
3. Trochanters
Finally, move to the greater and lesser trochanters. These should be followed carefully. Any discontinuity, sharp angulation, or small separate fragment of bone may represent a displaced fracture or avulsion fracture.
Review area checklist
Let’s summarise the above. Below you’ll find a checklist including the PANAPS RING mnemonic to help you when you next review a pelvic X-Ray.
| Projection | Mnemonic | Review area | Notes |
|---|---|---|---|
| AP | Soft tissue | Zoom out and look for asymmetry, swelling or gas locules. | |
| P | Pubic rami | Trace the superior and inferior pubic rami looking for fractures. | |
| A | Acetabulum | Trace the acetabular roof, iliopectineal and ilioischial lines. | |
| N | Neck of femur | Zoom up and look carefully for a lucent line, sclerotic line, break in cortex or angled trabeculae. | |
| A | Avulsion sites | Look closely for a fragment of bone around classic avulsion sites. | |
| P | Pedicles and lumbar spine | Don’t miss lumbar spine pathology. | |
| S | Sacro-iliac joints | Look for widening, narrowing, sclerosis or ankylosis. | |
| RING | Pelvic ring and obturator foramina | Follow the rings looking for a break that could mean a fracture. | |
| Final screen | Zoom out looking for a bone lesion or fracture you may have missed. | ||
| Lateral | Femoral neck | Look or a lucent line that could mean a fracture. | |
| Femoral head and acetabulum | Check alignment and look for a fracture. | ||
| Trochanters | Ensure no fracture or avulsion. |