Assessing pulmonary oedema
On chest X-Ray
Introduction
Pulmonary oedema is something every medical professional needs to recognise. Chest X-rays are quick and widely available, but the findings can be subtle and easy to miss if you’re not sure what to look for.
In this article, we walk through a real case and break down the key imaging features step by step. You’ll learn how to spot classic signs like Kerley B lines and the bat wing pattern, understand why fluid builds up in the lungs, and use the ABCDE approach to interpret X-rays with more confidence.
Case introduction
A 70-year-old male presents with breathlessness: have a look at his PA chest X-Ray. Let’s go through the case and have a think about pulmonary oedema.
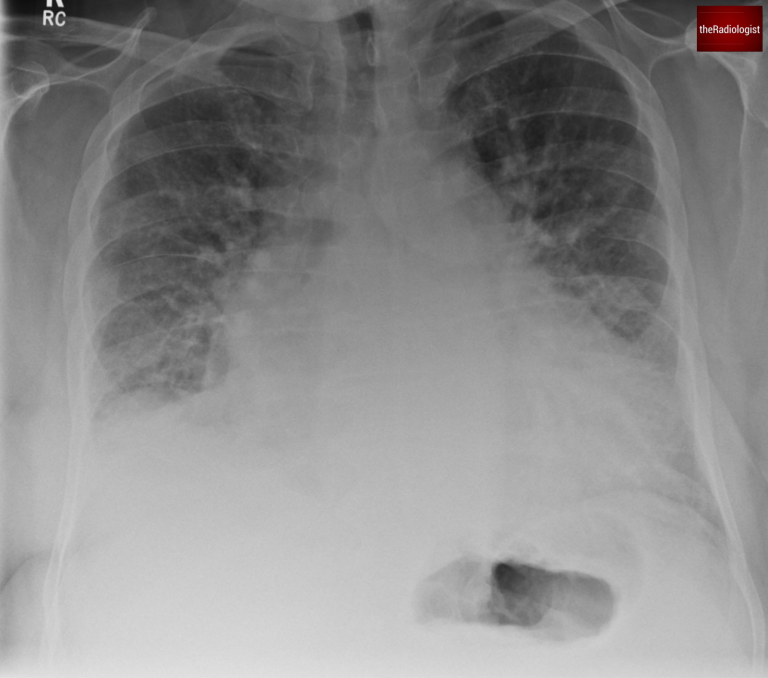
PA view of a chest X-Ray of a male in his 70s
Video explanation
Here is a video explanation of this case: click full screen in the bottom right corner to make it big. If you prefer though I go through this in the text explanation below.
What is pulmonary oedema?
Pulmonary oedema is the accumulation of extravascular fluid in the lungs. This can occur due to various mechanisms, but the most common cause is cardiogenic pulmonary oedema, often stemming from left heart failure. Non-cardiogenic causes include:
- Air embolism
- Neurogenic pulmonary oedema
- Reperfusion injuries
- Transfusion-related pulmonary oedema
How does this extravascular fluid build up?
Three key factors govern the movement of fluid between capillaries and interstitial spaces:
- Hydrostatic Pressure:
- Pressure exerted by blood within the capillaries forces fluid into the interstitial space.
- Increased hydrostatic pressure, as seen in left heart failure, leads to pulmonary oedema.
- Oncotic Pressure:
- Pressure exerted by plasma proteins like albumin pulls fluid back into capillaries.
- Decreased oncotic pressure, such as in hypoalbuminemia, allows more fluid to leak out.
- Capillary Permeability:
- The integrity of the vessel wall determines how easily fluid and proteins can escape.
- Direct damage to the alveoli or capillaries (e.g., ARDS) increases permeability, contributing to oedema.
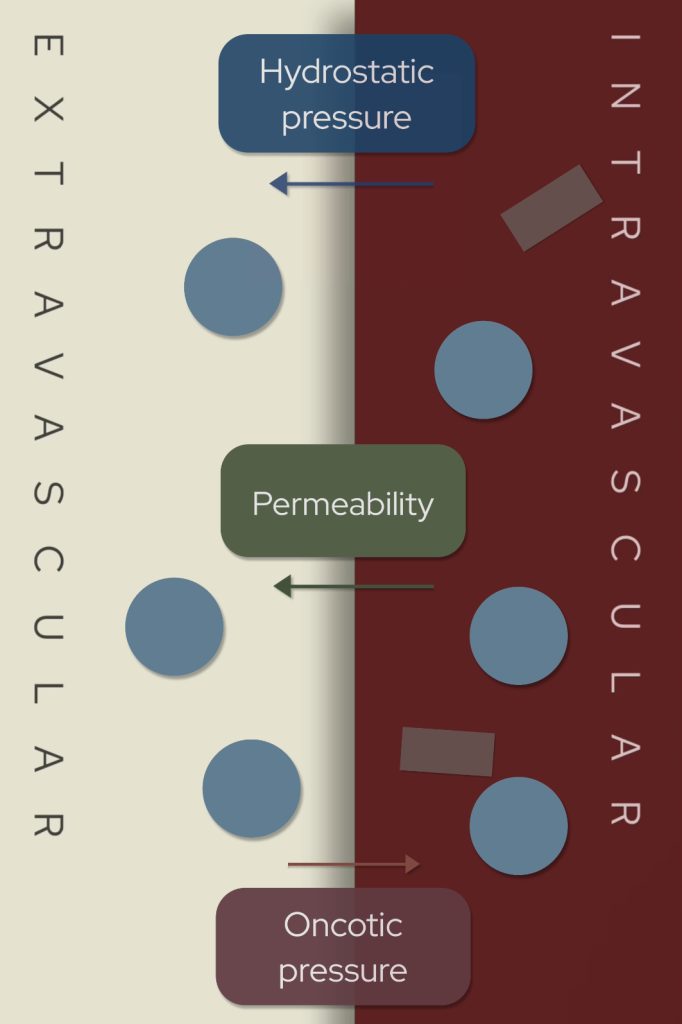
Increased hydrostatic pressure, increased permeability and reduced oncotic pressure can all lead to increased extravascular fluid and pulmonary oedema.
Pulmonary oedema on a chest X-Ray
Pulmonary oedema has a classic appearance on chest X-Ray. Let’s explore the key findings:
Vascular Redistribution
- Blood is redistributed to the upper lobe veins, causing them to dilate.
- This produces the antler sign, a hallmark of vascular congestion.
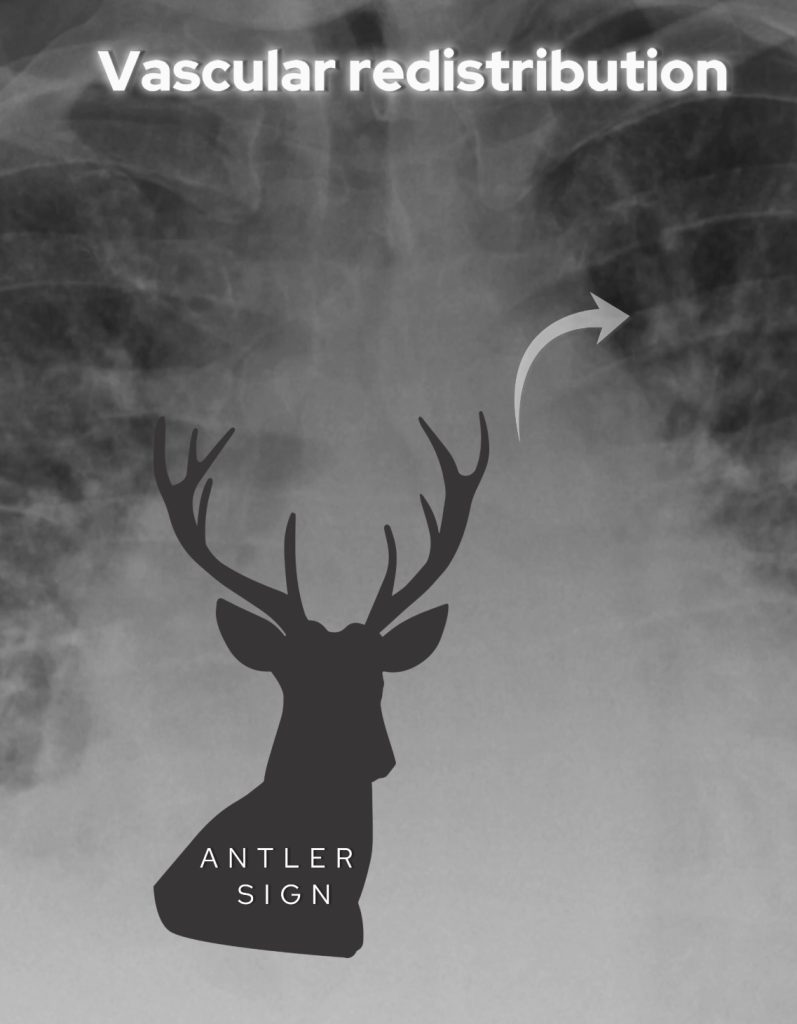
Look for dilated upper lobe veins – the ‘antler’ sign
Interstitial Oedema:
- Thickening of bronchial walls, also known as peribronchial cuffing.
- Loss of airway definition creates a hazy appearance.
- Kerley B lines, horizontal lines at the lung bases, indicate interstitial thickening.
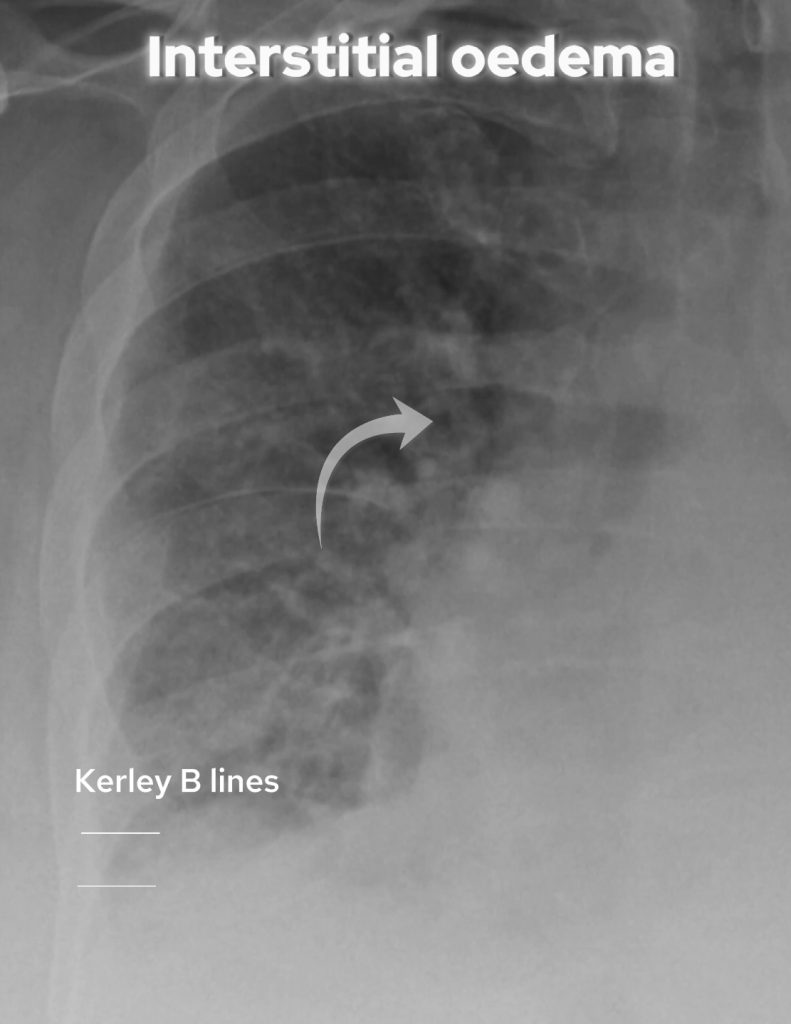
Look for thickening of bronchial walls and loss of definition of the airways. Kerley B lines were not present in this case but are seen as horizontal lines at the lung base reflecting interstitial thickening.
Alveolar Oedema:
- Fluid leaks into alveoli, causing fluffy opacities with air bronchograms.
- Rapid fluid accumulation can produce a bat wing pattern, central and bilateral.

Look for ‘fluffy’ alveolar oedema
Pleural Effusions:
- Fluid collects in the pleural spaces, blunting the costophrenic angles.
- Pleural fluid in cardiogenic oedema is a transudate, distinguished from exudates seen in infections or malignancies.
Other instances
- When fluid accumulation is rapid you may get the classic ‘bat wing’ appearance like the X-Ray below.
- Also note in cases of mitral regurgitation, the jet is directed towards the right sided superior pulmnonary vein and so severe mitral regurgitation can present with just right upper zone consolidation on chest X-Ray.
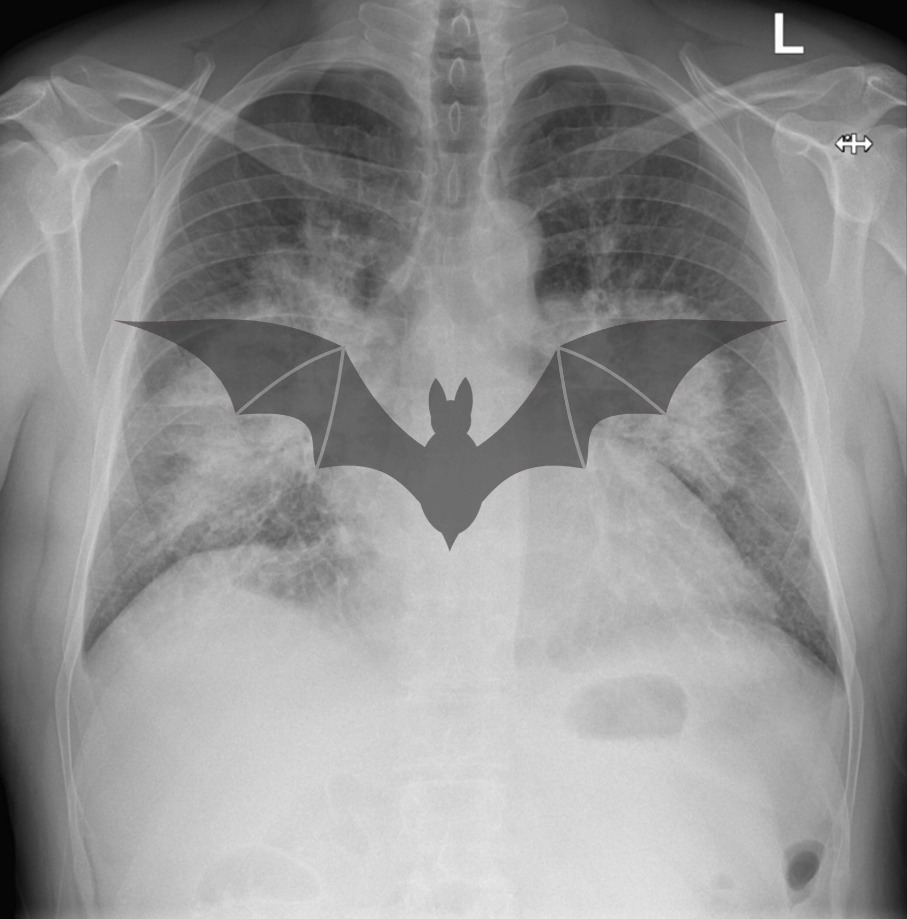
In this separate case there is rapid fluid accumulation leading to a classic bat wing appearance of pulmonary oedema.
Pulmonary oedema mnemonic
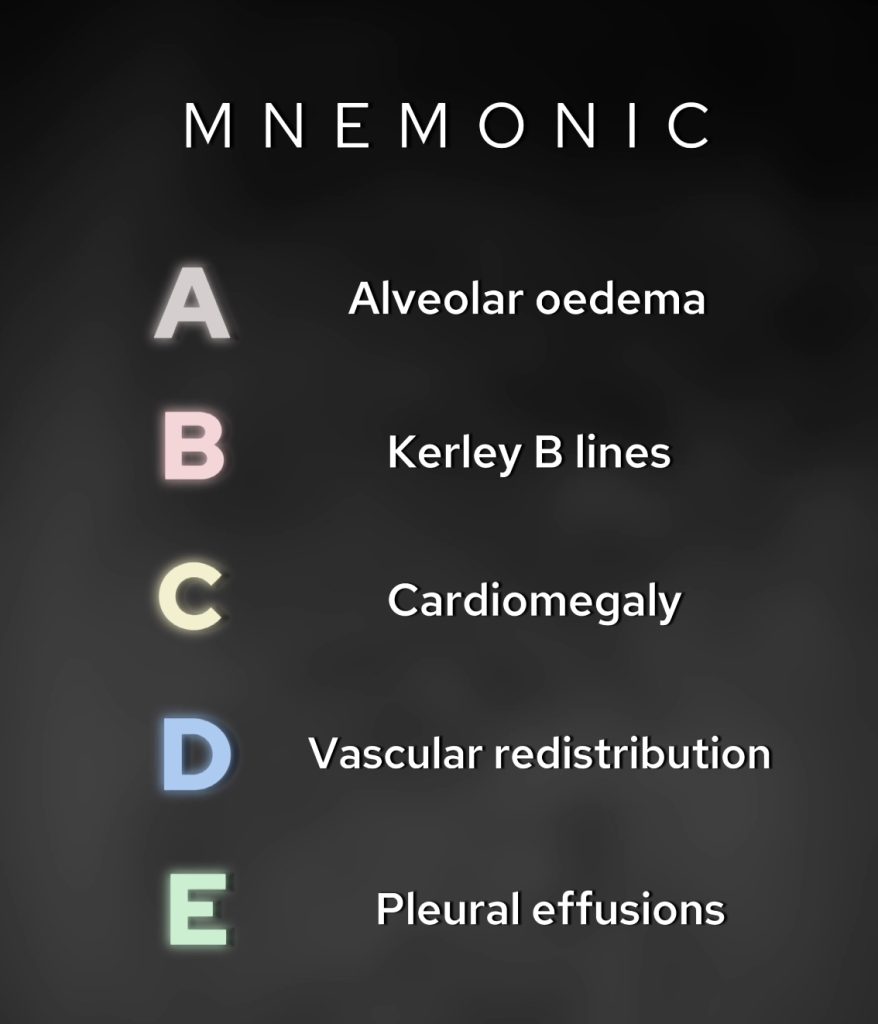
Here’s a handy mnemonic I’ve remembered since my days at med school about the findings of pulmonary oedema on chest X-Ray:
- A: Alveolar oedema (bilateral consolidation).
- B: Kerley B lines (interstitial thickening).
- C: Cardiomegaly (more common in cardiogenic cases).
- D: Vascular redistribution (dilated upper lobe veins).
- E: Effusions (bilateral blunting of angles).
DIAGNOSIS
In this patient, the findings are consistent with cardiogenic pulmonary oedema, caused by left ventricular dysfunction secondary to ischaemic heart disease.
We see vascular redistribution, interstitial oedema, and alveolar oedema on the X-ray.
Classifying pulmonary oedema
Pulmonary oedema can be classified into four categories based on the underlying mechanism:
- Hydrostatic Oedema:
- Most common, usually secondary to left heart failure.
- Permeability Oedema (without alveolar damage):
- Occurs in drug reactions or air embolism.
- CT may show more ground-glass opacity than hydrostatic oedema.
- Mixed Oedema:
- Combines hydrostatic and permeability mechanisms.
- Examples include high-altitude, neurogenic, reperfusion, or re-expansion oedema.
- Permeability Oedema (with alveolar damage):
- Seen in ARDS, caused by insults like severe pneumonia or pancreatitis.
- X-ray appearances may mimic cardiogenic oedema, but ARDS does not respond to diuresis and often results in lung fibrosis.
KEY POINTS
Don’t forget the ABCDE mnemonic for signs of pulmonary oedema – this is something I have been using since medical school and still use it to this day as a Consultant Radiologist.
Remember pulmonary oedema can be treated quickly and X-Ray features can resolve quickly (unless pneumonia and ARDS) so a short interval follow up X-Ray can help differentiate if things are difficult to interpret clinically.